Knee pain is a widespread complaint, often brushed aside as a mere consequence of aging or an active lifestyle. But when that occasional twinge becomes a persistent ache, it could be more than just wear and tear—it might signal knee osteoarthritis (OA). This condition is a leading cause of chronic knee pain worldwide, significantly affecting mobility and quality of life.
Osteoarthritis isn’t just about bones rubbing together; it’s a complex joint disorder influenced by age, weight, genetics, and lifestyle choices. Understanding its causes and effects is the first step in managing this common yet often misunderstood condition.
More Than Just a Twinge: Understanding the Basics
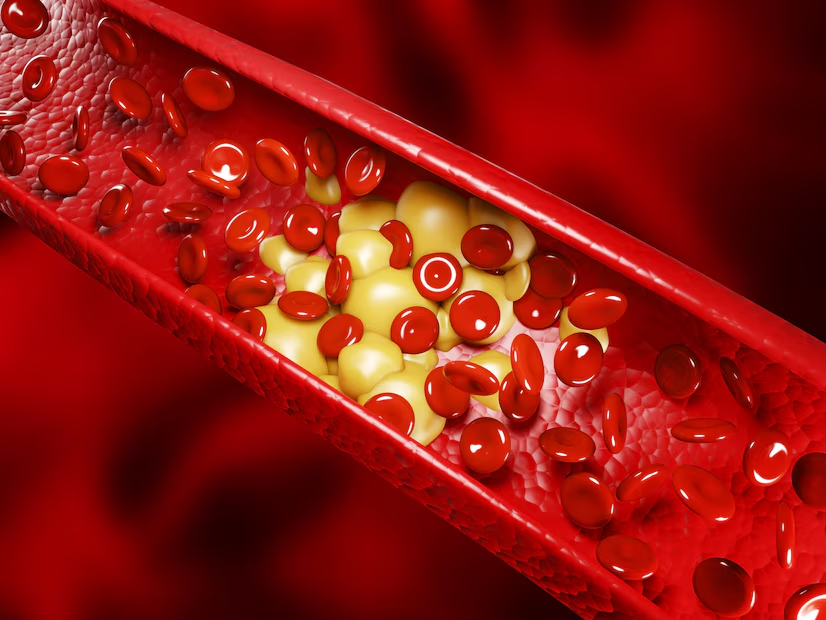
Knee osteoarthritis is a degenerative joint disease where the cartilage cushioning the ends of the bones gradually wears down. As the cartilage erodes, bones can start rubbing against each other, causing pain, swelling, stiffness, and reduced joint mobility. In advanced cases, bone spurs (osteophytes) may form, exacerbating discomfort and limiting movement.
This form of arthritis is classified into two types:
- Primary Osteoarthritis: Often age-related, developing without an obvious injury or condition.
- Secondary Osteoarthritis: Linked to an identifiable cause, such as injury, obesity, or a medical condition like rheumatoid arthritis.
While osteoarthritis can affect any joint, the knees bear the brunt due to their role in weight-bearing and movement.
Why Do Knees Age Faster Than We’d Like?
The knees are marvels of engineering, supporting our weight, enabling motion, and absorbing impact during activities like walking, running, and jumping. However, this constant workload makes them particularly vulnerable to wear and tear over time. Several factors accelerate the aging process of knees:
- Repetitive Stress: Years of bending, twisting, and heavy use can strain knee joints, gradually breaking down cartilage.
- Obesity: Excess weight increases the load on knees, with each additional pound putting approximately four extra pounds of pressure on the joints.
- Injuries: Previous knee injuries, such as ligament tears or fractures, can make joints more susceptible to early degeneration.
- Muscle Weakness: Weak quadriceps or hamstrings can destabilize the knee, increasing wear on the joint surfaces.
- Genetics: Some people are genetically predisposed to osteoarthritis, inheriting weaker cartilage or other risk factors.
Though aging is inevitable, understanding the mechanics behind knee degeneration helps emphasize the importance of prevention and early management. By adopting joint-friendly habits and seeking timely medical advice, you can slow the progression of knee osteoarthritis and maintain an active lifestyle.
The Anatomy of a Worn-Out Joint
The knee is a complex marvel of biological engineering, designed to endure years of movement, impact, and load-bearing. However, as we age or subject our knees to excessive stress, the intricate components of the joint begin to falter. The smooth, painless motion we take for granted can give way to stiffness, discomfort, and grinding sensations. Let’s break down the key elements of a knee joint and how they change when osteoarthritis takes hold.
Cartilage: The Cushion That’s Running Out
Cartilage is the soft, rubbery tissue that covers the ends of bones in the knee joint, acting as a shock absorber and providing a frictionless surface for movement. In a healthy knee, cartilage ensures smooth gliding as you bend and straighten your leg.
When osteoarthritis sets in, this essential cushion begins to wear away. The loss of cartilage leads to:
- Reduced Shock Absorption: Without enough cushioning, even routine movements like walking or standing can become painful.
- Increased Friction: The bones start rubbing against each other, causing pain and inflammation.
- Visible Symptoms: The joint may appear swollen or feel stiff, especially after periods of inactivity.
Once cartilage is lost, it doesn’t regenerate naturally, making early intervention crucial to preserving joint health.
Synovial Fluid: When the Lubrication Stops Working
Synovial fluid, a thick, gel-like substance within the knee joint, serves as a natural lubricant and nutrient supplier for cartilage. It helps reduce friction during movement and absorbs impact.
In osteoarthritis:
- Fluid Quality Decreases: The synovial fluid loses its ability to effectively lubricate the joint, leading to increased wear and tear.
- Inflammation Rises: Damaged cartilage releases enzymes and proteins that irritate the joint lining, further degrading the fluid’s quality.
- Dry Joint Effect: Without adequate lubrication, movement becomes less smooth, contributing to the characteristic stiffness of osteoarthritis.
Treatment approaches like viscosupplementation aim to restore the quality of synovial fluid, offering some relief for affected joints.
Bones, Joints, and That Grinding Sound
When cartilage thins and synovial fluid deteriorates, the underlying bones in the knee joint are left exposed. This leads to the hallmark grinding or creaking sound—known as crepitus—associated with osteoarthritis.
Here’s what happens to the bones and joints:
- Bone-on-Bone Contact: As cartilage erodes, bones rub directly against each other, causing pain and further damage.
- Bone Spurs: The body attempts to repair itself by forming extra bone, called osteophytes, around the joint. These spurs can cause additional pain and restrict movement.
- Joint Deformity: Over time, the knee joint may lose its natural alignment, leading to a bow-legged or knock-kneed appearance.
These changes not only cause pain but also limit mobility, making it increasingly difficult to perform everyday activities.
Understanding the anatomy of a worn-out knee joint highlights why osteoarthritis is more than just a “sign of aging.” It’s a condition that demands proactive care to maintain function and minimize pain.
Spotting the Signs: From Mild Annoyance to Daily Struggle
Knee pain often starts subtly—a twinge here, an ache there. But as osteoarthritis progresses, these minor discomforts can evolve into constant challenges, affecting every aspect of daily life. Recognizing the early signs of knee osteoarthritis can help you take timely action to slow its progression and manage symptoms effectively. Let’s explore how your knees communicate their distress and the warning signs you shouldn’t ignore.
Is That Pain Just Fatigue or Something More Serious?
Not all knee pain is created equal. While occasional discomfort after a long day or intense activity may be harmless, persistent or worsening pain could indicate an underlying issue.
In osteoarthritis:
- Activity-Related Pain: Pain often flares up during or after activity, especially if you’ve been walking, climbing stairs, or standing for long periods.
- Weather Sensitivity: Many individuals notice their knee pain worsening during cold or damp weather.
- Rest Pain: As the condition progresses, pain may persist even when you’re at rest, particularly at night.
These patterns distinguish osteoarthritis-related pain from temporary fatigue or muscle soreness, signaling the need for a closer look at your joint health.
Morning Stiffness: A Clue Your Knees Are Speaking
A stiff knee upon waking is one of the earliest signs of osteoarthritis. This symptom, often brushed off as “getting older,” is a red flag for joint dysfunction.
What to watch for:
- Short Duration: Morning stiffness typically lasts less than 30 minutes, unlike inflammatory conditions like rheumatoid arthritis, where stiffness lasts longer.
- Difficulty Starting Movement: Getting out of bed or beginning your day may feel sluggish until your joints “warm up.”
- Recurrent Stiffness: Stiffness can also occur after periods of inactivity, such as sitting for extended periods.
If morning stiffness becomes a regular occurrence, it’s time to pay attention to your knees’ needs.
Swelling, Clicking, and Buckling: The Other Red Flags
Beyond pain and stiffness, osteoarthritis brings a host of other symptoms that can interfere with daily activities and mobility.
- Swelling: Inflammation in the joint lining or the build-up of synovial fluid can cause visible swelling around the knee.
- Clicking or Popping Sounds: Known as crepitus, these sounds occur when damaged cartilage and bones grind against each other during movement.
- Buckling or Instability: Weak or damaged knee structures may cause the joint to “give out,” leading to sudden falls or difficulty bearing weight.
These signs are indicators that the joint is struggling to function properly, often marking the progression from mild to moderate or severe osteoarthritis.
The Causes You Didn’t See Coming
Knee osteoarthritis doesn’t happen overnight. It’s the result of a combination of factors—some obvious, others less so—that gradually take a toll on your joints. While aging is the most common culprit, several other influences may accelerate the degeneration process. Understanding these causes can empower you to take preventative steps and reduce your risk of developing osteoarthritis.
Blame It on Time: Age and Wear-and-Tear
As we grow older, our joints naturally experience wear and tear. The cartilage that cushions the bones in our knees thins with time, and the body’s ability to repair joint tissues diminishes.
Age-related changes include:
- Reduced Cartilage Resilience: Cartilage becomes less elastic and more prone to damage over time.
- Declining Joint Fluid: The synovial fluid that lubricates the joint may decrease in volume or quality.
- Accumulated Micro-Damage: Decades of walking, running, and other activities gradually add up, even without major injuries.
While aging is inevitable, staying active, maintaining a healthy lifestyle, and protecting your joints can help slow this natural process.
Weight Matters: Extra Pounds, Extra Pressure
Excess body weight is one of the most significant risk factors for knee osteoarthritis. The knees bear the brunt of your body weight, with every extra pound adding approximately four pounds of pressure to the joints.
The impact of obesity on knee health includes:
- Increased Joint Stress: Higher weight accelerates the wear-and-tear process.
- Inflammatory Effects: Fat tissue releases chemicals that promote joint inflammation, worsening cartilage damage.
- Earlier Onset: Overweight individuals often develop osteoarthritis at a younger age compared to those with a healthy weight.
Weight management is a critical step in preventing and managing osteoarthritis, helping to reduce stress on the knees and improve overall joint health.
Injuries That Leave a Lingering Legacy
Knee injuries from sports, accidents, or overuse can increase the risk of osteoarthritis later in life. Even when the immediate damage appears to heal, the joint may be left vulnerable to long-term degeneration.
Common injury-related causes include:
- Ligament Tears (e.g., ACL injuries): These can destabilize the knee, leading to uneven wear on the cartilage.
- Meniscus Tears: Damage to this cushioning tissue can accelerate joint breakdown.
- Fractures: A break in the knee joint can alter its alignment and biomechanics, contributing to osteoarthritis.
Rehabilitating injuries thoroughly and protecting the joint during recovery are crucial to minimizing the risk of future complications.
Genetics, Gender, and Why Women Are More Vulnerable
Some people are predisposed to osteoarthritis due to their genetic makeup. If a close family member has experienced knee osteoarthritis, your risk may be higher. Additionally, women are more likely than men to develop this condition, especially after menopause.
Key contributing factors:
- Hormonal Changes: Estrogen levels drop after menopause, which may affect cartilage health.
- Joint Alignment: Women tend to have wider hips, which can alter the biomechanics of the knees and increase stress on the joint.
- Genetic Factors: Certain inherited traits, like weaker cartilage or bone structure, can predispose individuals to osteoarthritis.
Understanding your risk factors, including family history and hormonal influences, allows you to take proactive measures to support joint health through diet, exercise, and preventive care.
Lifestyle or Luck? Risk Factors That Tip the Scale
When it comes to knee osteoarthritis, the line between unavoidable circumstances and modifiable lifestyle choices isn’t always clear. While genetics and aging play a role, your day-to-day habits and activities can significantly influence the health of your knees. From your choice of footwear to your workplace duties, subtle factors often tip the scale, increasing the risk of osteoarthritis. Let’s explore the ways lifestyle and luck intertwine in the development of this common condition.
High-Heels, Low Chairs, and Bad Posture: The Everyday Culprits
Sometimes, it’s the small choices we make daily that have a lasting impact on our knees. Seemingly innocuous habits, such as wearing the wrong shoes or sitting improperly, can place undue stress on the joints over time.
- High Heels: Stylish but harmful, high heels shift your body weight forward, increasing pressure on the knee joint and accelerating cartilage wear.
- Low Chairs: Sitting in low, soft chairs can strain your knees when getting up, particularly if your muscles are weak or the joint is already inflamed.
- Poor Posture: Misaligned hips, back, or knees due to bad posture redistributes weight unevenly, leading to added strain on specific areas of the joint.
Making small adjustments—like choosing supportive footwear, practicing good posture, and using ergonomically designed furniture—can go a long way in protecting your knees.
Occupational Hazards: Jobs That Punish the Knees
Your profession may demand more from your knees than you realize. Jobs that involve repetitive movements, heavy lifting, or prolonged kneeling can place excessive stress on the joint, increasing the likelihood of osteoarthritis.
- Physically Demanding Jobs: Construction workers, athletes, and laborers often face joint strain due to repetitive impacts and weight-bearing activities.
- Prolonged Kneeling or Squatting: Occupations like gardening, plumbing, or flooring frequently require extended periods of knee flexion, which accelerates cartilage degradation.
- Repetitive Motion: Assembly line workers or those with similar repetitive tasks may develop “wear spots” in their cartilage from continuous, focused stress.
If your job is knee-intensive, regular stretching, using protective gear, and taking breaks can help mitigate damage.
When Exercise Hurts: Overuse Without Protection
Exercise is vital for overall health, but overdoing it—especially without proper form or protection—can harm your knees instead of helping them. High-impact activities, excessive repetition, or poor technique can wear down the joint faster than it can recover.
- High-Impact Sports: Running, basketball, or tennis can subject your knees to repeated stress and trauma, especially on hard surfaces.
- Overuse Injuries: Activities like cycling or weightlifting without proper rest or technique may strain tendons and ligaments, destabilizing the knee joint.
- Lack of Protective Measures: Skipping warm-ups, wearing improper footwear, or ignoring pain can exacerbate joint damage over time.
Balancing exercise with adequate rest, focusing on low-impact activities, and strengthening the muscles around your knees can help protect your joints while staying active.
Debunking Myths About Osteoarthritis
Osteoarthritis (OA) is one of the most misunderstood joint conditions, often clouded by myths and misconceptions. These myths can prevent people from taking proactive steps to manage their symptoms or even seeking help in the first place. By separating fact from fiction, you can better understand osteoarthritis and make informed decisions about your joint health.
“It’s Just Old Age” – Why That’s Not Entirely True
One of the most pervasive myths about osteoarthritis is that it’s simply an inevitable part of getting older. While age is a risk factor, it’s not the sole cause of OA.
Here’s the reality:
- Young People Can Get OA Too: Osteoarthritis can develop in younger individuals, especially those with injuries, genetic predispositions, or certain lifestyle factors.
- Not Everyone Develops OA: Many people live into old age without significant joint issues, proving that OA is not an automatic outcome of aging.
- Other Factors Play a Role: Obesity, previous joint injuries, repetitive stress, and even gender can influence the likelihood of developing osteoarthritis.
By addressing these risk factors, you can reduce your chances of developing OA, regardless of your age.
Does Weather Really Worsen Arthritis Pain?
Many people with osteoarthritis report that their symptoms worsen during cold or damp weather, leading to the widespread belief that weather directly affects joint pain. But does science support this claim?
What we know:
- No Clear-Cut Evidence: While some studies suggest a link between weather changes and arthritis pain, the connection is inconsistent and not well-understood.
- Barometric Pressure: Shifts in barometric pressure may affect joint tissues, particularly if they’re already inflamed or swollen, potentially causing discomfort.
- Personal Perception: Individuals may associate weather changes with pain due to heightened sensitivity or personal experiences.
While weather may influence how your joints feel, it’s unlikely to be the root cause of increased arthritis pain. Dressing warmly, staying active indoors, and using heat therapy can help manage symptoms during colder months.
Exercise Is Bad for Pain – Or Is It?
The belief that exercise is harmful for people with osteoarthritis is a damaging myth that prevents many from reaping its benefits. Contrary to this misconception, regular physical activity is one of the best ways to manage OA.
The truth about exercise and osteoarthritis:
- Strengthens Support Structures: Exercise builds muscles around the joint, improving stability and reducing strain on the knee.
- Increases Flexibility: Gentle stretching and low-impact activities enhance joint mobility and reduce stiffness.
- Reduces Pain: Movement encourages the production of synovial fluid, lubricating the joint and easing discomfort.
However, it’s essential to approach exercise wisely:
- Choose low-impact activities like swimming, cycling, or walking.
- Avoid high-impact exercises if they worsen your symptoms.
- Work with a physical therapist to develop a personalized exercise plan.
By staying active and informed, you can debunk the myth that rest is always best and embrace movement as a powerful tool for managing osteoarthritis.
Clearing up these misconceptions allows for better management and a more positive outlook on living with osteoarthritis. Knowledge is power—especially when it comes to your health.
How Does It Feel? The Day in the Life of Someone with Knee OA
Living with knee osteoarthritis (OA) is an ongoing challenge that affects more than just physical mobility. It’s a daily battle with discomfort, limitations, and emotional strain. To truly understand the impact of this condition, it’s important to walk in the shoes of someone navigating their day with knee OA.
The Morning Shuffle: Stiffness and Mobility Struggles
For many people with knee OA, mornings begin with a struggle to get moving. Upon waking, stiffness in the knees can make even the smallest movements feel laborious.
Here’s what mornings often bring:
- Painful First Steps: The initial steps out of bed can feel like moving through molasses, with sharp or dull pain accompanying each movement.
- Limited Range of Motion: Knees may feel “locked” or difficult to bend, requiring time and gentle stretching to regain functionality.
- Fatigue Before the Day Begins: Starting the day with discomfort can set a tone of frustration, making even simple tasks feel daunting.
Incorporating morning stretches or heat therapy can help alleviate this stiffness, but the struggle remains an ever-present reminder of OA’s impact.
Climbing Stairs: A Test of Willpower and Strength
For someone with knee OA, stairs transform from a routine part of the day into a significant obstacle. The physical effort required to ascend or descend can be overwhelming, especially when pain flares up.
What climbing stairs feels like:
- Sharp, Localized Pain: Weight-bearing activities, such as climbing stairs, can trigger sharp pain in the knees, particularly around the kneecap or joint edges.
- Instability: The fear of the knee “giving out” can make each step feel precarious, requiring extra concentration and support.
- Exhaustion: The effort to complete even a single flight can leave the person drained, both physically and emotionally.
Many find themselves avoiding stairs altogether, leading to further restrictions on their mobility and lifestyle.
The Emotional Toll: From Frustration to Isolation
The physical challenges of knee OA are compounded by the emotional burden it places on individuals. The constant presence of pain and the inability to engage in previously enjoyed activities can take a significant toll on mental health.
Common emotional experiences include:
- Frustration: Simple tasks that once required no thought—like walking, cooking, or running errands—become sources of irritation and helplessness.
- Social Withdrawal: Embarrassment over mobility aids or difficulty keeping up with others can lead to avoidance of social situations.
- Fear of the Future: Concerns about further joint deterioration and potential loss of independence weigh heavily on the mind.
Addressing the emotional aspect of knee OA is just as important as managing physical symptoms. Support groups, therapy, and open communication with loved ones can provide much-needed relief and connection.
Diagnosis: When to Seek Help and What to Expect
Knee osteoarthritis (OA) can sneak up gradually, with early symptoms that are easy to dismiss. However, delaying a diagnosis can mean missing the window for effective management. Knowing when to seek help and what to expect during the diagnostic process is key to taking control of your joint health.
Early Warning Signs That Shouldn’t Be Ignored
Recognizing the early signs of knee OA can make a significant difference in managing the condition. These subtle clues are often mistaken for normal fatigue or overuse, but they may be red flags of an underlying problem.
Signs to watch for:
- Persistent Pain: Aching or soreness in the knee that lingers beyond activity or worsens over time.
- Morning Stiffness: Difficulty bending or straightening the knee after waking, lasting up to 30 minutes.
- Swelling or Warmth: Occasional swelling or warmth around the joint, even without significant activity.
- Grinding Sensation: A feeling of grating or grinding when moving the knee, often accompanied by audible clicking or popping sounds.
If these symptoms persist or worsen, it’s time to consult a healthcare provider for a proper assessment.
X-rays, MRIs, and the Truth About Joint Space
When you visit a doctor for knee pain, imaging tests are often part of the diagnostic process. Each type of imaging provides unique insights into the condition of your joint.
- X-rays: The most common initial test, X-rays reveal changes in the bone structure, such as narrowing of the joint space, bone spurs, or alignment issues. While effective at identifying moderate to severe OA, X-rays may not detect early cartilage damage.
- MRI (Magnetic Resonance Imaging): An MRI offers a detailed view of soft tissues like cartilage, tendons, and ligaments. This is particularly useful for diagnosing early-stage OA or ruling out other conditions like meniscus tears.
- Joint Space Insight: Narrowed joint space on imaging is a hallmark of OA, indicating cartilage loss. However, the degree of narrowing doesn’t always correlate with the severity of symptoms—some patients with mild joint space loss may experience significant pain, and vice versa.
Discussing imaging results with your doctor can help you understand the extent of your joint damage and plan appropriate treatment.
What Your Doctor Might Miss: The Importance of a Thorough Exam
While imaging is important, a comprehensive diagnosis of knee OA requires more than just looking at test results. A thorough clinical exam can uncover subtleties that imaging might miss.
Key aspects of a proper examination include:
- Range of Motion Testing: Evaluating how well your knee moves can reveal stiffness or instability.
- Physical Palpation: Feeling the joint for warmth, swelling, or tenderness provides insights into inflammation.
- Gait Analysis: Observing how you walk can identify compensatory movements or uneven weight distribution.
- Discussion of Symptoms: Describing your pain patterns, activity limitations, and how symptoms affect your daily life is crucial for an accurate diagnosis.
Doctors who focus solely on imaging may overlook important functional impairments or the emotional toll of OA. Don’t hesitate to advocate for a comprehensive evaluation if you feel your symptoms are being underestimated.
Treatments Beyond the Painkillers
Managing knee osteoarthritis (OA) involves more than just popping painkillers. While medications can offer short-term relief, addressing the root causes and symptoms of OA requires a multifaceted approach. Fortunately, there are several treatment options that go beyond medication, focusing on strengthening the joint, reducing inflammation, and improving mobility. Here, we break down these treatments to help you find what works best for your knees.
The Ice and Heat Debate: When to Use What
Both ice and heat are commonly recommended for easing pain and inflammation in knee OA, but using them effectively requires understanding when and how each works.
- Ice: Ice is most beneficial during flare-ups or acute inflammation. Cold therapy reduces swelling and numbs the pain by constricting blood vessels and limiting fluid buildup around the joint. Use ice for 15-20 minutes, several times a day, especially after activity that worsens your symptoms.
- Heat: Heat helps to relax tight muscles and improve blood flow to the area. It’s ideal for soothing stiffness or chronic pain, especially when the joint feels tense or sore after periods of inactivity. A warm compress or heating pad can be used for 15-20 minutes to ease discomfort before engaging in activity or stretching.
The key to the ice and heat debate is knowing when to use each one: ice for swelling and inflammation, heat for stiffness and muscle tension. Both can be valuable tools in managing OA symptoms.
Physical Therapy: Strengthening Without Straining
Physical therapy is one of the most effective non-surgical treatments for knee OA. By targeting the muscles that support the knee joint, physical therapy helps reduce strain on the damaged cartilage and restores mobility.
What physical therapy offers:
- Strengthening Exercises: Focused on strengthening the quadriceps, hamstrings, and calf muscles, these exercises provide better support to the knee joint, reducing pain and improving function.
- Flexibility and Mobility Training: Stretching and flexibility exercises help improve joint range of motion and reduce stiffness.
- Pain-Reducing Techniques: A physical therapist may teach you techniques to reduce stress on the knee, such as adjusting your gait or using assistive devices.
A customized physical therapy plan can significantly improve strength and flexibility while avoiding the strain that could exacerbate OA symptoms.
Braces and Supports: Are They Worth It?
Knee braces and supports are commonly used to provide stability, alleviate pain, and reduce further damage to the knee joint. But are they really effective for OA?
- Knee Braces: For people with knee OA, especially those with mild to moderate symptoms, a knee brace can help stabilize the joint and reduce pain during activity. Unloader braces are designed to shift pressure away from the damaged part of the knee, which can improve function and reduce discomfort.
- Knee Sleeves and Supports: These offer compression, which can reduce swelling and provide support to the knee without restricting movement. They are often used for mild cases of OA or as an additional layer of protection during exercise.
While knee braces and supports can be beneficial, they should be used alongside other treatments like physical therapy for long-term improvement. They’re a temporary solution to help with mobility and pain management, not a cure for OA.
Over-the-Counter Supplements: Fact vs. Hype
Many people turn to over-the-counter supplements like glucosamine, chondroitin, or turmeric in hopes of alleviating knee OA symptoms. While some of these supplements have gained popularity, the evidence supporting their effectiveness is mixed.
- Glucosamine and Chondroitin: These are among the most commonly used supplements for OA. Some studies suggest that glucosamine and chondroitin may help slow cartilage deterioration and reduce pain in some individuals, but results are not consistent.
- Turmeric and Omega-3 Fatty Acids: Turmeric has anti-inflammatory properties, and omega-3 fatty acids (found in fish oil) are known to reduce joint inflammation. Some people with OA report significant improvement with these supplements.
- Hyaluronic Acid: Available as an oral supplement or injected directly into the knee, hyaluronic acid can improve joint lubrication and reduce pain.
Though these supplements may provide relief for some individuals, they should not replace medical treatment. Always talk to your doctor before starting a new supplement, as some may interact with other medications or have side effects.
When Medications Enter the Picture
For many people with knee osteoarthritis (OA), the pain and inflammation can become difficult to manage with just lifestyle changes and physical therapy. When symptoms worsen or don’t improve with non-invasive treatments, medications can play an important role in providing relief. However, understanding when and how to use them is crucial, as medications are typically most effective when combined with other treatment approaches. Here, we explore the role of medications in OA management, including pain relievers, anti-inflammatories, and injections.
Pain Relievers: Quick Fix or Long-Term Solution?
Pain relievers, such as acetaminophen and over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), are often the first line of defense against knee OA pain. These medications can provide quick relief, but they come with important considerations regarding their long-term use.
- Acetaminophen: Often recommended as a first step for mild to moderate pain, acetaminophen (Tylenol) is effective in managing discomfort without affecting inflammation. However, it does not treat the underlying cause of the pain, and overuse can lead to liver damage.
- NSAIDs (e.g., ibuprofen, naproxen): These drugs not only alleviate pain but also reduce inflammation, which is a common symptom of knee OA. However, they carry risks such as stomach ulcers, gastrointestinal bleeding, and kidney damage if taken frequently or for long periods.
While pain relievers offer temporary relief, they do not address the root cause of OA and should not be relied upon as a long-term solution. If over-the-counter pain relievers are used regularly, it’s essential to consult a doctor about alternative treatments and potential risks.
Anti-Inflammatories and Their Side Effects
Anti-inflammatory medications (like NSAIDs) are a cornerstone of managing knee OA pain. While effective in reducing swelling and pain, long-term use of these drugs can come with significant side effects.
- Gastrointestinal Issues: Chronic use of NSAIDs can cause stomach ulcers, indigestion, or bleeding. This is why it’s essential to take them with food or under the supervision of a healthcare provider.
- Kidney Problems: NSAIDs can affect kidney function, especially in people with pre-existing kidney conditions or those who use them long-term.
- Heart Risks: Prolonged use of certain NSAIDs can increase the risk of heart problems, including heart attack or stroke.
Due to these risks, doctors typically recommend using anti-inflammatories sparingly and may suggest alternatives like physical therapy, injections, or lifestyle modifications for managing OA symptoms long-term.
Injections: From Cortisone to Hyaluronic Acid – Do They Help?
When oral medications no longer provide sufficient relief, injections can offer a more targeted approach to treating knee OA. Two common types of injections are corticosteroids (cortisone) and hyaluronic acid, both designed to reduce pain and improve function.
- Corticosteroid Injections: These injections deliver powerful anti-inflammatory medications directly into the knee joint. They can provide quick relief from pain and swelling, especially during flare-ups. However, repeated use of corticosteroids can potentially weaken the joint, and relief may be temporary (lasting weeks to months).
- Hyaluronic Acid Injections: Hyaluronic acid is a naturally occurring substance that helps lubricate the joints. These injections are meant to improve the knee’s cushioning and reduce friction, offering pain relief and improved joint mobility. While they don’t stop the progression of OA, many people find significant benefit in terms of pain relief and function. However, they may require multiple injections to be effective, and results can vary.
Injections can offer significant relief, but they are not a cure. They’re most effective when used in conjunction with other treatments like physical therapy and weight management. Additionally, they may not be suitable for all patients, and a doctor’s guidance is necessary to determine the best approach based on the severity of OA.
Surgical Solutions: The Last Resort
When all non-surgical treatments for knee osteoarthritis (OA) fail to provide sufficient relief and quality of life becomes increasingly difficult to maintain, surgery may be considered as a last resort. While surgery can be life-changing and offer substantial pain relief, it is typically only recommended when conservative options have been exhausted. Understanding the different surgical options, the recovery process, and the consequences of delaying surgery can help you make informed decisions about the future of your knee health.
Partial vs. Total Knee Replacement: What’s the Difference?
Knee replacement surgery is one of the most common surgeries for severe OA. There are two main types of knee replacement procedures: partial knee replacement and total knee replacement. Both aim to alleviate pain and restore function, but they differ in terms of the extent of the surgery.
- Partial Knee Replacement (Unicompartmental Knee Arthroplasty): In a partial knee replacement, only the damaged portion of the knee is replaced, leaving the healthy parts of the joint intact. This procedure is typically recommended when OA is isolated to just one area of the knee, such as the inside, outside, or front part of the joint. The recovery time is generally quicker, and patients may experience less pain post-surgery. However, partial replacement may not be suitable for those with widespread joint damage.
- Total Knee Replacement (Total Knee Arthroplasty): A total knee replacement involves removing the damaged cartilage and bone from the entire knee joint and replacing it with artificial components. This surgery is usually recommended for patients with extensive damage throughout the knee or when other treatments have failed to provide relief. Total knee replacement provides a more comprehensive solution, but it comes with a longer recovery period and a higher risk of complications than partial knee replacement.
Choosing between partial and total knee replacement depends on the extent of the damage to the knee, the patient’s overall health, and the recommendation of the orthopedic surgeon.
The Road to Recovery: Life After Surgery
Recovery from knee replacement surgery can take time, patience, and dedication. Whether you undergo a partial or total knee replacement, there are certain steps you’ll need to follow to maximize your recovery and regain mobility.
- Hospital Stay and Immediate Post-Surgery Care: After surgery, you’ll typically stay in the hospital for a few days. Pain management, antibiotics to prevent infection, and early mobilization are key parts of the recovery process. You will likely start physical therapy soon after surgery to begin restoring range of motion.
- Physical Therapy: Physical therapy plays a crucial role in helping you regain strength, flexibility, and function in your knee. You’ll work with a therapist to perform exercises that will strengthen the muscles around the knee and improve movement. Consistency is essential for a successful recovery.
- Returning to Normal Activities: Most people can resume light activities, like walking or driving, within a few weeks. However, high-impact activities such as running or jumping should be avoided for several months or longer, depending on your surgeon’s advice. Full recovery may take 6-12 months, though you may feel significant improvement much sooner.
Staying positive and following your healthcare team’s guidance will help ensure the best possible recovery.
What Happens If You Delay Surgery Too Long?
Delaying knee surgery can have consequences, especially if OA is severely affecting the knee joint. While it’s natural to hesitate about surgery, putting it off for too long may lead to worsening symptoms and a more complicated recovery.
- Increased Pain and Disability: As the cartilage continues to wear away, the knee joint may become more unstable, leading to chronic pain, stiffness, and difficulty walking or standing for long periods.
- Decreased Mobility and Function: The longer OA goes untreated, the more likely it is that joint deformity and loss of function will occur, making surgery more difficult and potentially less effective.
- Muscle Atrophy: When knee pain limits movement, the muscles around the knee may weaken over time. This makes recovery from surgery more difficult and may slow the rehabilitation process.
While surgery should always be considered carefully, delaying it too long can lead to a more challenging path to recovery. Consulting with an orthopedic surgeon early on can help you determine the best time for surgery and prevent the complications associated with delaying the procedure.
Lifestyle Tweaks That Make a Difference
While medical treatments can help manage knee osteoarthritis (OA) symptoms, lifestyle changes are essential for long-term joint health and mobility. Small adjustments to your daily routine can make a significant difference in managing knee pain, improving function, and slowing down the progression of OA. By adopting joint-friendly workouts, tweaking your diet, and focusing on weight management, you can take control of your knee health and enhance your overall well-being.
“Joint-Friendly” Workouts: Swimming, Yoga, and Walking Right
Exercise is crucial for managing OA, but it’s important to choose activities that minimize stress on the knee joint while building strength and flexibility. Some of the best options for knee OA include low-impact exercises that promote joint health without aggravating symptoms.
- Swimming: Swimming is a fantastic low-impact exercise that provides a full-body workout while being gentle on the knees. The buoyancy of the water supports your body, reducing stress on the joints and allowing for a range of motion. Swimming laps or doing water aerobics can help strengthen the muscles around the knee, improve flexibility, and boost cardiovascular health.
- Yoga: Yoga is another excellent choice for those with knee OA. The practice focuses on gentle stretching, strengthening, and balance, all of which can help improve knee mobility and reduce stiffness. Certain yoga poses can help open the hips, strengthen the thighs, and relieve tension in the knee joint. Just be sure to work with an instructor who can modify poses to suit your needs.
- Walking Right: Walking is a natural, weight-bearing activity that’s great for strengthening the muscles around the knee. However, proper walking form is essential to avoid putting extra strain on your knees. Focus on maintaining good posture, walking with a natural stride, and avoiding hard surfaces that may exacerbate joint pain. If needed, consider using walking aids, like a cane or walking poles, to take some of the load off your knee.
Incorporating these joint-friendly exercises into your routine can improve knee function and reduce pain, helping you maintain an active lifestyle without causing further damage to the joint.
Diet Do’s and Don’ts: Foods That Ease Inflammation
What you eat can have a significant impact on the health of your joints. Certain foods can help reduce inflammation, support cartilage health, and manage OA symptoms, while others may worsen inflammation. A diet rich in anti-inflammatory foods can complement your treatment plan and contribute to better knee function.
- Do Eat:
- Omega-3 Fatty Acids: Found in fatty fish like salmon, sardines, and mackerel, omega-3 fatty acids have powerful anti-inflammatory effects that can help reduce joint pain and stiffness.
- Antioxidant-Rich Fruits and Vegetables: Berries, cherries, spinach, and kale are high in antioxidants that help reduce inflammation and protect joint health.
- Whole Grains: Foods like oatmeal, quinoa, and brown rice are rich in fiber and have anti-inflammatory properties. They can help manage weight and provide steady energy without causing blood sugar spikes.
- Turmeric and Ginger: Both spices have been shown to have natural anti-inflammatory effects, making them great additions to your diet. Try adding turmeric to soups or smoothies and ginger to teas or stir-fries.
- Don’t Eat:
- Processed Foods and Sugars: Processed snacks, sugary drinks, and refined carbohydrates can contribute to inflammation, worsening OA symptoms. Avoiding these foods can help reduce the overall inflammation in the body.
- Saturated and Trans Fats: Found in fatty meats, fried foods, and some processed snacks, these fats can contribute to inflammation. Opt for healthier fats like those found in nuts, seeds, and olive oil.
- Excessive Alcohol: Alcohol can increase inflammation and worsen symptoms for some people with OA. Moderating alcohol intake can help reduce flare-ups and improve overall health.
By focusing on a diet rich in anti-inflammatory foods and reducing those that promote inflammation, you can help support joint health and reduce OA symptoms.
Weight Loss Without Knee Pain: Practical Tips for a Healthier You
Excess weight places additional stress on the knees, accelerating cartilage breakdown and worsening osteoarthritis symptoms. Losing weight can significantly alleviate pain, improve mobility, and slow the progression of OA. However, it’s important to approach weight loss carefully to avoid exacerbating knee pain.
- Start Slowly: Sudden, intense physical activity can stress the knees, so begin with low-impact exercises like walking, swimming, or cycling. Gradually increase intensity as your fitness improves.
- Focus on Nutrition: Weight loss is largely driven by diet. By eating a balanced, nutrient-dense diet and controlling portion sizes, you can create a calorie deficit while still providing your body with the nutrients it needs.
- Strength Training: Building muscle helps support the knee joint and can reduce the strain on the cartilage. Consider incorporating strength training exercises into your routine, focusing on the muscles that support the knee, such as the quadriceps and hamstrings.
- Monitor Progress: Track your weight loss journey, but also monitor how your knees feel as you lose weight. Many people find that even a modest reduction in weight leads to noticeable improvements in pain and mobility.
Losing weight in a sustainable, low-impact way can have a profound effect on knee OA. By combining a healthy diet, low-impact exercise, and strength training, you can reduce joint pain and support long-term knee health.
Living with Knee Osteoarthritis: A New Normal
Knee osteoarthritis (OA) is more than just a physical condition—it can affect every aspect of your life, from your daily routine to your emotional well-being. Learning how to manage OA requires a shift in perspective, recognizing that while the condition may be part of your life, it doesn’t have to define it. Finding new ways to live with the disease can help you regain control, maintain your mental health, and achieve a sense of normalcy. By focusing on mental health, seeking support, and setting achievable goals, you can navigate the challenges of living with knee OA.
Mental Health Matters: Coping with Chronic Pain
Chronic pain from knee osteoarthritis can take a heavy toll on mental health. The constant discomfort, combined with limited mobility, can lead to feelings of frustration, anxiety, and even depression. It’s important to recognize that mental health is just as crucial as physical health when managing OA.
- Acknowledge the Emotional Impact: The daily struggle with knee pain can lead to feelings of hopelessness or irritability. Acknowledging these feelings is the first step toward coping with them. It’s essential to be kind to yourself and recognize that dealing with OA is a long-term journey.
- Mindfulness and Relaxation Techniques: Practices like meditation, deep breathing, or progressive muscle relaxation can help reduce stress and alleviate the emotional burden of living with chronic pain. These techniques can improve your ability to manage pain and promote overall well-being.
- Therapy and Counseling: For some people, seeking professional support through therapy can provide valuable tools for managing the mental health challenges that come with chronic pain. Cognitive-behavioral therapy (CBT) is particularly effective in helping individuals reframe negative thoughts and develop coping strategies.
Taking care of your mental health is essential for maintaining a positive outlook and managing the challenges of knee osteoarthritis. By addressing emotional well-being, you can foster resilience and improve your quality of life.
Joining Support Groups and Communities: Why You’re Not Alone
One of the most powerful ways to cope with knee OA is by connecting with others who understand what you’re going through. Support groups and communities provide an opportunity to share experiences, ask questions, and find encouragement from people facing similar challenges.
- The Power of Shared Experiences: In support groups, you can hear firsthand how others manage their symptoms, what treatments have worked for them, and how they handle the emotional aspects of OA. These shared experiences can provide comfort, hope, and practical advice that might be hard to find elsewhere.
- Online Communities and Forums: If in-person support groups aren’t an option, online communities can be a great way to connect with others. Websites, social media platforms, and dedicated forums offer a wealth of information, support, and a space to share your own journey.
- Building Emotional Support Networks: Connecting with family and friends who understand your condition can also make a huge difference. Encourage open conversations about what you need from them, whether it’s emotional support or assistance with day-to-day tasks.
Being part of a supportive community can combat feelings of isolation and provide valuable resources, making the journey of living with knee OA feel less daunting.
Setting Realistic Goals: Achieving Small Wins Every Day
Living with knee osteoarthritis means adapting to a new normal, but that doesn’t mean giving up on goals or dreams. Setting realistic, achievable goals can help you stay motivated and maintain a sense of accomplishment.
- Focus on Small, Achievable Goals: Rather than focusing on big, distant goals, break them down into smaller, more manageable steps. For example, instead of aiming to run a marathon, set a goal to walk a certain distance each day or to improve your knee strength with specific exercises.
- Celebrate Progress, Not Perfection: Every step forward is a victory. Celebrate your successes, no matter how small, and recognize the effort you’ve put into maintaining your health. Whether it’s increasing your daily step count, completing a physical therapy session, or simply having a pain-free moment, every win matters.
- Adjust Goals as Needed: Your goals may evolve as your knee OA progresses, and that’s okay. Being flexible with your expectations allows you to adapt to changes in your health and adjust your approach when necessary.
By setting realistic goals, you can continue to move forward in your journey with knee OA, maintaining a sense of control and achievement even on tough days.
Living with knee osteoarthritis requires a mindset shift—acknowledging that your life may look different, but it can still be fulfilling. By focusing on mental health, seeking support from others, and setting realistic goals, you can find new ways to adapt, thrive, and maintain a high quality of life despite the challenges of OA.