Defining Gluten Sensitivity
Gluten sensitivity, also known as non-celiac gluten sensitivity (NCGS), refers to a condition where individuals experience gastrointestinal discomfort or other symptoms after consuming gluten, without having celiac disease or a wheat allergy. Unlike celiac disease, which involves an autoimmune response, and wheat allergy, which involves an allergic reaction, gluten sensitivity is still not fully understood. People with gluten sensitivity might experience symptoms like bloating, diarrhea, or fatigue, but there is no definitive test for it.
Gluten Sensitivity vs. Celiac Disease vs. Wheat Allergy
Understanding the differences between gluten sensitivity, celiac disease, and wheat allergy is essential in diagnosing and managing these conditions.
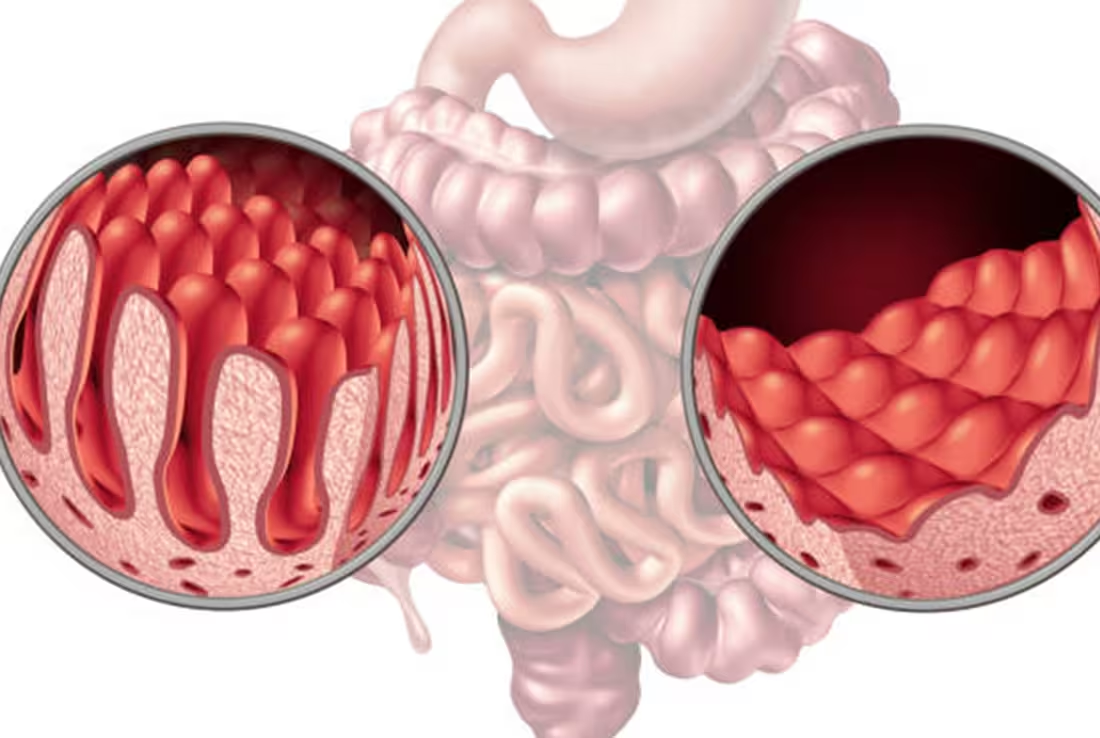
Celiac Disease
Celiac disease is an autoimmune disorder where consuming gluten damages the lining of the small intestine. This damage can lead to nutrient malabsorption, digestive issues, and other long-term health problems. It is diagnosed through blood tests and biopsies.
Wheat Allergy
Wheat allergy is an allergic reaction to proteins found in wheat, including gluten. This condition can cause severe symptoms, such as difficulty breathing, swelling, or anaphylaxis, and is typically diagnosed through allergy testing.
Gluten Sensitivity
Unlike the other two conditions, gluten sensitivity does not involve immune system activation or damage to the intestine. Symptoms may mimic those of celiac disease but do not cause permanent damage to the digestive system. Diagnosis is often through the process of elimination, as there are no specific tests for gluten sensitivity.
Importance of Understanding Gluten Sensitivity
Understanding gluten sensitivity is crucial for proper diagnosis and management. Without a clear understanding, individuals might be misdiagnosed with other conditions like irritable bowel syndrome or be overlooked entirely. Knowing the distinction between gluten sensitivity, celiac disease, and wheat allergy can help people make informed decisions about their diet and lifestyle. Early recognition can improve quality of life by preventing unnecessary discomfort and ensuring a healthier, gluten-free or gluten-limited diet if necessary.
What is Gluten?
Gluten is a group of proteins found in wheat and related grains, such as barley and rye. It is responsible for the elasticity and texture of dough, helping it rise and maintain its shape. When flour is mixed with water, gluten forms a network of proteins that gives the dough its chewy texture. This protein is crucial in many baked goods, giving them structure and preventing them from crumbling. In the human diet, gluten is often the main protein source in products like bread, pasta, and baked goods.
Explanation of Gluten and Its Role in Food
Gluten plays a fundamental role in food production, especially in baking. It gives dough its characteristic elasticity, allowing it to trap air bubbles during the leavening process. This is what helps bread rise, giving it a soft and chewy texture. In addition to its structural role, gluten also helps retain moisture in baked goods, contributing to their freshness. It also plays a role in the texture of processed foods like soups and sauces, acting as a stabilizer or thickener.
Common Sources of Gluten
Gluten is commonly found in a variety of foods, especially those made from wheat, barley, and rye. Common sources include bread, pasta, cakes, cookies, crackers, and pastries. It can also be present in processed foods where it might be used as a stabilizing or thickening agent, such as in sauces, soups, or salad dressings. Gluten is also found in some cereals, snacks, and even certain condiments or seasonings. People with gluten sensitivity or celiac disease must be vigilant about checking food labels to avoid accidental consumption.
Gluten in Different Types of Grains
Gluten is found in several grains, but the most common sources are wheat, barley, and rye. In wheat, the primary gluten proteins are gliadin and glutenin, which combine to form gluten when mixed with water. Barley contains a form of gluten that is similar to wheat gluten, and rye also contains a similar protein structure. Other grains like oats may be contaminated with gluten during processing, but oats themselves do not contain significant amounts of gluten. People who are sensitive to gluten must avoid not only these grains but also any cross-contamination from other gluten-containing products.
Understanding Gluten Sensitivity
Gluten sensitivity, also referred to as non-celiac gluten sensitivity (NCGS), is a condition where individuals experience symptoms similar to those of celiac disease or a wheat allergy after consuming gluten. However, unlike celiac disease, gluten sensitivity does not cause damage to the intestine, and unlike wheat allergy, it does not trigger an immune-mediated allergic response. The exact mechanisms behind gluten sensitivity remain unclear, and it is diagnosed primarily through the process of exclusion, where other conditions like celiac disease and wheat allergy are ruled out.
Overview of Non-Celiac Gluten Sensitivity (NCGS)
Non-celiac gluten sensitivity is characterized by gastrointestinal and extra-intestinal symptoms triggered by gluten consumption, but without the autoimmune response or damage seen in celiac disease. Individuals with NCGS often experience discomfort such as bloating, diarrhea, fatigue, and headaches, but these symptoms resolve once gluten is eliminated from the diet. There are no specific biomarkers to diagnose NCGS, and its diagnosis is often made after ruling out celiac disease and wheat allergy. Research on NCGS is still ongoing to better understand its underlying causes and effective treatment methods.
How Gluten Sensitivity Differs from Celiac Disease and Wheat Allergy
Gluten sensitivity differs from celiac disease in that it does not involve an autoimmune response or damage to the intestinal lining. While celiac disease triggers an immune reaction that causes inflammation and damage to the small intestine, gluten sensitivity does not cause these physical changes, although symptoms may be similar. Gluten sensitivity also differs from a wheat allergy, which is an allergic reaction to the proteins in wheat, including gluten, but typically involves immune system activation that can lead to severe symptoms such as anaphylaxis. In contrast, gluten sensitivity symptoms are usually less severe and do not cause life-threatening reactions.
Symptoms of Gluten Sensitivity
The symptoms of gluten sensitivity can vary widely and affect different parts of the body. Common gastrointestinal symptoms include bloating, abdominal pain, diarrhea, and gas. Extra-intestinal symptoms may include fatigue, headaches, joint pain, and brain fog. These symptoms typically appear after consuming gluten-containing foods and can improve when gluten is removed from the diet. However, unlike celiac disease, these symptoms do not cause permanent damage to the intestines, and there are no specific blood tests to confirm the condition.
Causes and Mechanisms Behind Gluten Sensitivity
The exact causes and mechanisms behind gluten sensitivity are still unclear. Unlike celiac disease, where the immune system triggers an autoimmune response, gluten sensitivity does not involve clear immune system activation. Some theories suggest that gluten sensitivity may be related to an altered gut microbiome, where an imbalance in gut bacteria could contribute to digestive symptoms. Another possibility is that the immune system could be involved, but it may not result in the same autoimmune response seen in celiac disease. However, more research is needed to understand the biological mechanisms at play and why some individuals develop gluten sensitivity while others do not.
Symptoms of Gluten Sensitivity
Gluten sensitivity can manifest through a wide range of symptoms that affect various systems in the body. These symptoms are often triggered by the consumption of gluten-containing foods and can vary in severity. While gastrointestinal issues are the most common, gluten sensitivity can also lead to neurological, skin, musculoskeletal, and emotional symptoms. It’s important to note that these symptoms generally improve when gluten is removed from the diet, though the exact mechanism behind gluten sensitivity is still not fully understood.
Digestive Symptoms (Bloating, Diarrhea, Constipation)
One of the most common symptoms of gluten sensitivity is digestive discomfort. Many individuals report experiencing bloating, abdominal pain, and changes in bowel movements. This may include diarrhea, where the stool is loose and watery, or constipation, which involves difficulty passing stool. These symptoms often mimic those of other gastrointestinal conditions like irritable bowel syndrome (IBS), making it challenging to diagnose gluten sensitivity without ruling out other potential causes. Some individuals may also experience gas and cramping after consuming gluten.
Neurological Symptoms (Headaches, Brain Fog, Fatigue)
In addition to digestive symptoms, gluten sensitivity can also affect the nervous system. Common neurological symptoms include frequent headaches or migraines, which may occur alongside other discomforts. Brain fog, a condition where individuals experience difficulty concentrating or thinking clearly, is also frequently reported. Fatigue is another common symptom, where individuals feel unusually tired or drained, even after a full night’s sleep. These neurological symptoms can be disruptive to daily life and are often a significant reason why people seek diagnosis and treatment for gluten sensitivity.
Skin Issues (Rashes, Itchiness)
Gluten sensitivity can also lead to skin issues, although these are less commonly discussed. Some individuals experience rashes, redness, or irritation on their skin. These rashes may be accompanied by itchiness, and the affected areas can range from small patches to more widespread outbreaks. The exact connection between gluten and skin symptoms is still not entirely understood, but it is thought that the inflammation caused by gluten may contribute to these reactions. Conditions such as dermatitis herpetiformis are related to celiac disease but are sometimes seen in people with gluten sensitivity as well.
Musculoskeletal Pain and Joint Issues
Musculoskeletal symptoms such as joint pain, muscle aches, and stiffness are also commonly reported by individuals with gluten sensitivity. These symptoms can affect various joints, including the knees, elbows, and wrists, and may be particularly noticeable in the morning or after long periods of inactivity. The exact cause of these symptoms is not entirely clear, but it is thought that gluten may trigger an inflammatory response in the body, leading to pain and discomfort in the muscles and joints. These symptoms can often mimic conditions such as rheumatoid arthritis, but they tend to improve with dietary changes.
Emotional and Psychological Symptoms
Gluten sensitivity may also impact emotional and psychological well-being. Many individuals report feeling irritable, anxious, or even depressed when they consume gluten. This may be related to the inflammatory effects of gluten on the body or the stress caused by ongoing physical symptoms. The link between gluten sensitivity and mental health symptoms is still being explored, but there is evidence to suggest that diet and gut health play significant roles in mood regulation. Improving symptoms by removing gluten from the diet may lead to noticeable improvements in mood and overall psychological health.
Diagnosis of Gluten Sensitivity
Diagnosing gluten sensitivity can be challenging due to the lack of specific tests and the overlap of symptoms with other gastrointestinal and autoimmune conditions. Since gluten sensitivity is diagnosed primarily by excluding other conditions, it requires a thorough process that involves medical tests and an evaluation of symptoms. Understanding the diagnosis process is crucial for individuals who suspect they may have gluten sensitivity, as it helps differentiate this condition from celiac disease, wheat allergy, or other disorders.
Medical Tests and Procedures (Blood Tests, Biopsy, etc.)
Currently, there are no specific blood tests or procedures that can definitively diagnose gluten sensitivity. However, doctors may perform a variety of tests to rule out other conditions that present similar symptoms. Blood tests for celiac disease are often the first step, as they can identify specific antibodies associated with this autoimmune disorder. A biopsy of the small intestine may also be performed to assess any damage caused by celiac disease. Additionally, tests for wheat allergy may be conducted to eliminate the possibility of an allergic reaction to wheat. Since gluten sensitivity does not have its own diagnostic test, these tests help ensure an accurate diagnosis.
Process of Exclusion (Ruling out Celiac Disease and Wheat Allergy)
The process of diagnosing gluten sensitivity typically involves a process of exclusion. The first step is to rule out celiac disease, which can be done through blood tests and, in some cases, a biopsy of the small intestine. If celiac disease is ruled out, the next step is to test for a wheat allergy, which may involve skin or blood tests to detect allergic reactions. Once both celiac disease and wheat allergy are excluded, and if a patient continues to experience symptoms after consuming gluten, a diagnosis of gluten sensitivity may be considered. This process often involves detailed medical history-taking, symptom tracking, and careful observation of the patient’s response to a gluten-free diet.
Challenges in Diagnosing Gluten Sensitivity
Diagnosing gluten sensitivity presents several challenges due to the absence of clear biomarkers and the overlap of symptoms with other conditions. Many symptoms of gluten sensitivity, such as abdominal pain, bloating, fatigue, and headaches, are also seen in other gastrointestinal disorders, including irritable bowel syndrome (IBS), lactose intolerance, and other food sensitivities. This makes it difficult to identify gluten sensitivity without ruling out these other possibilities. Additionally, some individuals may have mild or intermittent symptoms, which can further complicate diagnosis. The process often requires the patient’s cooperation in tracking symptoms and making dietary adjustments to assess improvement.
The Role of a Medical Professional in Diagnosis
A medical professional plays a crucial role in diagnosing gluten sensitivity. Due to the complex nature of the condition and the need to rule out other possible causes of symptoms, a healthcare provider should be involved in overseeing the diagnostic process. A doctor or specialist, such as a gastroenterologist or allergist, will conduct a thorough evaluation, including blood tests, medical history reviews, and symptom tracking. They will help differentiate between gluten sensitivity, celiac disease, and wheat allergy by performing appropriate tests and guiding patients through the exclusion process. Medical professionals may also provide advice on dietary changes, including the elimination of gluten, and monitor the patient’s response to ensure an accurate diagnosis and proper management of the condition.
Treatment and Management of Gluten Sensitivity
The treatment and management of gluten sensitivity primarily involve dietary changes, with a focus on avoiding gluten-containing foods. Since gluten sensitivity does not involve the permanent damage seen in celiac disease, it is typically managed by eliminating gluten from the diet. Along with dietary adjustments, managing cross-contamination, maintaining a balanced diet, and addressing potential nutritional deficiencies are crucial aspects of treatment. Lifestyle adjustments, including stress management, also play an important role in managing symptoms and improving overall well-being.
Gluten-Free Diet as the Primary Treatment
The primary treatment for gluten sensitivity is adopting a strict gluten-free diet. This means avoiding all foods that contain gluten, which is found in wheat, barley, rye, and any products made from these grains. A gluten-free diet can significantly reduce or eliminate symptoms such as bloating, diarrhea, fatigue, and headaches. People with gluten sensitivity are encouraged to choose naturally gluten-free foods, such as fruits, vegetables, meats, fish, legumes, and gluten-free grains like rice, quinoa, and corn. It is essential to read food labels carefully to ensure there is no hidden gluten, as it can be found in many processed and packaged foods.
Importance of a Balanced Diet for Gluten Sensitivity
While a gluten-free diet is essential for managing gluten sensitivity, it is equally important to maintain a balanced and nutritious diet. Gluten-free foods can sometimes lack certain nutrients, such as fiber, iron, and B vitamins, which are often found in gluten-containing grains. To ensure overall health, individuals with gluten sensitivity should incorporate a variety of nutrient-dense foods into their diet. This includes whole grains like quinoa, millet, and gluten-free oats, as well as fruits, vegetables, lean proteins, and healthy fats. A balanced diet can help prevent nutrient deficiencies and support optimal health while adhering to a gluten-free lifestyle.
Managing Cross-Contamination in a Gluten-Free Diet
One of the challenges of a gluten-free diet is preventing cross-contamination. Even small amounts of gluten can trigger symptoms in people with gluten sensitivity. Cross-contamination can occur when gluten-free foods come into contact with gluten-containing foods, either during preparation, cooking, or storage. To manage cross-contamination, individuals should be diligent about using separate utensils, cooking surfaces, and storage containers for gluten-free foods. It is also important to thoroughly clean surfaces, appliances, and dishes before using them for gluten-free cooking. Many people with gluten sensitivity also choose to eat foods that are certified gluten-free to ensure they are safe from contamination.
Supplementation and Nutritional Considerations
Individuals with gluten sensitivity may need to consider supplementation and nutritional adjustments to ensure they are meeting all of their dietary needs. Since a gluten-free diet can sometimes be low in certain nutrients, supplementation may be necessary to maintain health. Common supplements include calcium, vitamin D, iron, and B vitamins, which are often found in gluten-containing foods. Additionally, because gluten-free grains can be lower in fiber, some individuals may benefit from fiber supplements to support digestive health. A healthcare provider or dietitian can help assess any potential nutritional deficiencies and recommend appropriate supplements.
Lifestyle Adjustments and Stress Management
In addition to dietary changes, lifestyle adjustments can play a significant role in managing gluten sensitivity. Stress can exacerbate symptoms and trigger flare-ups, so practicing stress management techniques is essential. Techniques such as yoga, meditation, deep breathing exercises, and regular physical activity can help reduce stress levels and improve overall well-being. Adequate sleep and maintaining a healthy routine can also help manage symptoms and support the body’s ability to heal. Lifestyle modifications, along with a gluten-free diet, can provide relief from gluten sensitivity and enhance the quality of life.
Gluten-Free Diet: What to Eat and What to Avoid
A gluten-free diet is essential for managing gluten sensitivity, and it involves avoiding foods that contain gluten while focusing on naturally gluten-free options. Since gluten is found in many common foods, individuals with gluten sensitivity must become familiar with both the foods to avoid and the gluten-free alternatives available. Careful meal planning and understanding food labels are also crucial to ensure a safe and balanced diet. Below is an overview of what to eat and what to avoid on a gluten-free diet.
Foods that Contain Gluten
Gluten is primarily found in wheat, barley, rye, and foods made from these grains. Common foods that contain gluten include bread, pasta, cakes, cookies, crackers, pastries, and most cereals. Many processed foods also contain gluten as an ingredient or thickening agent, so it’s important to check labels for hidden sources of gluten, such as malt, modified food starch, and wheat flour. Foods such as beer, certain sauces, and packaged snacks may also contain gluten. People with gluten sensitivity should avoid these foods to prevent symptoms and discomfort.
Gluten-Free Grains and Alternatives
While many grains contain gluten, there are several naturally gluten-free grains and alternatives that individuals with gluten sensitivity can enjoy. These include rice, quinoa, corn, millet, buckwheat, and gluten-free oats. These grains can be used in a variety of dishes, such as salads, soups, and baked goods. Additionally, gluten-free flour options, such as rice flour, corn flour, and potato flour, can be used to replace wheat flour in baking. By incorporating these gluten-free grains and alternatives into the diet, individuals can enjoy a diverse and nutritious range of meals without compromising on flavor or texture.
Popular Gluten-Free Substitutes (Flours, Breads, Pastas)
There are numerous gluten-free substitutes available to replace traditional gluten-containing products. Gluten-free flours, such as almond flour, coconut flour, and chickpea flour, are commonly used in baking and cooking. These flours provide similar texture and structure to wheat flour and are suitable for making gluten-free cakes, cookies, and bread. Gluten-free breads and pastas are widely available in supermarkets, made from ingredients like rice flour, cornmeal, or quinoa. Many gluten-free pastas are also made from legume-based flours, such as lentil or chickpea flour, offering additional protein and fiber. While gluten-free substitutes can often replicate the taste and texture of their gluten-containing counterparts, experimenting with different products can help individuals find their preferred options.
Meal Planning for Gluten Sensitivity
Meal planning is an important aspect of managing gluten sensitivity, as it ensures that meals are both gluten-free and nutritionally balanced. When planning meals, individuals should focus on whole, unprocessed foods, such as fresh fruits, vegetables, lean proteins, and gluten-free grains. Incorporating a variety of gluten-free grains, vegetables, legumes, and proteins can help create well-rounded meals that provide essential nutrients. It’s also a good idea to prepare meals in advance to avoid the temptation of gluten-containing fast foods or convenience items. Meal planning may involve trying out new recipes, checking labels carefully, and ensuring that all kitchen equipment is free from gluten contamination. A well-thought-out meal plan can help individuals manage their condition effectively while enjoying delicious and satisfying meals.
Gluten-Free Labeling and Certification
Understanding gluten-free labeling is essential for anyone following a gluten-free diet. In many countries, including the U.S. and EU, products labeled as “gluten-free” must meet specific regulatory standards to ensure they contain fewer than 20 parts per million (ppm) of gluten. This is considered the threshold below which most individuals with gluten sensitivity can safely consume the product without triggering symptoms. Certified gluten-free products often bear a seal from an official certification body, such as the Gluten-Free Certification Organization (GFCO), which provides an additional level of assurance that the product meets gluten-free standards. It’s important for individuals to rely on trusted gluten-free labels and certifications when purchasing packaged foods to avoid accidental gluten consumption.
Living with Gluten Sensitivity
Living with gluten sensitivity requires ongoing vigilance and adjustments to daily routines, but it is entirely manageable with the right strategies. Coping with social situations, eating out, and traveling can pose unique challenges, but there are ways to navigate these experiences successfully. Additionally, managing the emotional and psychological aspects of living with gluten sensitivity is essential for overall well-being. Support networks and resources also play a critical role in providing guidance and encouragement.
Coping Strategies for Social Situations
Social situations, such as family gatherings, parties, or dining with friends, can be challenging for individuals with gluten sensitivity. One of the most effective coping strategies is to communicate openly with friends, family, and event hosts about dietary needs. Preparing and bringing gluten-free dishes to share can also ensure there are safe food options available. If attending a restaurant or catered event, it’s helpful to call ahead or review the menu online to identify gluten-free options or ask about the possibility of modifying dishes to be gluten-free. Staying proactive and educating others about gluten sensitivity can ease social situations and reduce the likelihood of accidental gluten exposure.
Eating Out and Traveling with Gluten Sensitivity
Eating out and traveling while managing gluten sensitivity requires careful planning. When dining out, it’s important to choose restaurants that offer gluten-free options or are knowledgeable about cross-contamination. Many restaurants now have gluten-free menus, or staff can provide information about how food is prepared and whether they can accommodate dietary restrictions. For travelers, packing gluten-free snacks and meals can help ensure access to safe food during long trips. It’s also a good idea to research gluten-free restaurants and grocery stores in the area beforehand. When traveling abroad, learning key phrases in the local language to explain dietary restrictions can be beneficial. Planning ahead can make dining out and traveling more enjoyable and less stressful.
Managing Mental Health with Gluten Sensitivity
Living with gluten sensitivity can sometimes lead to mental health challenges, such as stress, anxiety, and frustration, especially when dealing with symptoms or social pressures. It is important to recognize that these feelings are valid and can be managed with a combination of coping strategies. Practicing stress management techniques, such as mindfulness, yoga, or meditation, can help reduce anxiety related to dietary restrictions. Additionally, maintaining a positive outlook and focusing on the improvements in overall health and well-being from following a gluten-free diet can provide emotional support. For individuals experiencing significant mental health concerns, seeking professional support from a therapist or counselor who understands the challenges of living with dietary restrictions can be helpful.
Support Networks and Resources
Building a support network is crucial for individuals living with gluten sensitivity. Connecting with family, friends, or support groups can provide encouragement and help alleviate feelings of isolation. There are also online communities, forums, and social media groups where individuals with gluten sensitivity can share experiences, tips, and recipes. Support from healthcare professionals, including dietitians or gastroenterologists, is valuable for ongoing management of the condition. Resources such as gluten-free recipe websites, blogs, and cookbooks can offer inspiration and guidance for meal planning and food preparation. Support networks and resources provide essential emotional support and practical advice for managing life with gluten sensitivity.
The Controversy Around Gluten Sensitivity
The topic of gluten sensitivity has sparked ongoing debate within the medical community and among the general public. While many people experience relief from symptoms when adopting a gluten-free diet, others question whether gluten sensitivity is a legitimate condition or simply a trend. There are also concerns about overdiagnosis and the influence of media and public perception on the increasing number of individuals identifying as gluten-sensitive. Understanding the controversies surrounding gluten sensitivity is important for both those affected by it and the healthcare providers who manage it.
Debates About the Existence of Gluten Sensitivity
One of the key controversies surrounding gluten sensitivity is whether it is a legitimate medical condition. While celiac disease and wheat allergy have clear physiological mechanisms, gluten sensitivity lacks specific biomarkers or diagnostic tests, making it harder to validate as a distinct disorder. Some researchers argue that the symptoms attributed to gluten sensitivity could be caused by other conditions, such as irritable bowel syndrome (IBS), lactose intolerance, or psychological factors. Others contend that non-celiac gluten sensitivity (NCGS) is real but requires more research to fully understand its mechanisms and prevalence. As scientific studies continue to explore the condition, there remains uncertainty about how to definitively diagnose or classify gluten sensitivity.
The Role of the Media and Public Perception
The media plays a significant role in shaping public perception of gluten sensitivity. With the increasing popularity of gluten-free diets in recent years, many celebrities, influencers, and health experts have endorsed gluten-free living, which has led to a surge in the number of people self-diagnosing as gluten-sensitive. Media outlets often focus on the health benefits of gluten-free diets, sometimes without distinguishing between those with celiac disease, wheat allergies, or gluten sensitivity. This widespread exposure has raised awareness about gluten sensitivity but has also contributed to misconceptions and confusion about its true nature. As a result, people may feel pressured to adopt a gluten-free lifestyle, even if they don’t have a formal diagnosis of gluten sensitivity.
Is Gluten Sensitivity Overdiagnosed?
There is concern among some healthcare professionals that gluten sensitivity may be overdiagnosed, partly due to the influence of media coverage and the growing popularity of gluten-free diets. Many individuals self-diagnose based on symptoms like bloating, fatigue, or headaches, which are common in various conditions unrelated to gluten. In the absence of objective diagnostic tests, the process of diagnosing gluten sensitivity often involves excluding other potential causes, which can sometimes lead to a misdiagnosis. Additionally, some may adopt a gluten-free diet based on the belief that it will improve overall health, despite not having any specific gluten-related disorder. This has raised questions about whether gluten sensitivity is being identified more frequently than it should be, potentially leading to unnecessary dietary restrictions and treatments.
Addressing Myths and Misconceptions
There are several myths and misconceptions surrounding gluten sensitivity that contribute to its controversy. One common misconception is that gluten sensitivity is simply a fad or a psychological issue rather than a legitimate condition. Another myth is that gluten-free diets are inherently healthier, which is not necessarily true, as many gluten-free processed foods can be low in essential nutrients. Additionally, some people mistakenly believe that gluten sensitivity is only related to digestive issues, when in fact it can also affect the skin, joints, and even mental health. Addressing these myths is important to provide accurate information about gluten sensitivity and help people make informed decisions about their health. Educating the public about the complexity of gluten sensitivity and the need for proper diagnosis is crucial in dispelling misconceptions and ensuring effective management of the condition.
Gluten Sensitivity and Children
Gluten sensitivity in children presents unique challenges for both parents and healthcare providers. While children can experience similar symptoms to adults, such as digestive issues, fatigue, and skin problems, recognizing gluten sensitivity in children can be more difficult due to their limited ability to communicate or understand their symptoms. Managing gluten sensitivity in children requires special attention to diet, nutritional needs, and social considerations. Support for parents and caregivers is also essential to ensure children with gluten sensitivity can thrive while following a gluten-free diet.
Recognizing Gluten Sensitivity in Children
Recognizing gluten sensitivity in children can be difficult because the symptoms are often nonspecific and may overlap with other conditions. Common signs in children include stomachaches, bloating, diarrhea, constipation, and irritability. Some children may also experience neurological symptoms, such as difficulty concentrating or fatigue, while others might develop skin rashes or joint pain. Since these symptoms are similar to those of other common pediatric conditions, such as irritable bowel syndrome (IBS) or food allergies, a thorough evaluation by a healthcare professional is essential to rule out other potential causes. Parents and caregivers should be attentive to patterns in their child’s health and report symptoms to a pediatrician for further investigation.
Pediatric Gluten-Free Diet
Once gluten sensitivity is diagnosed in a child, the primary treatment is a gluten-free diet. This requires eliminating all sources of gluten, including wheat, barley, and rye, from the child’s meals and snacks. A pediatric gluten-free diet should be balanced and nutrient-dense to support the child’s growth and development. This includes offering a variety of gluten-free grains, such as rice, quinoa, and gluten-free oats, along with fruits, vegetables, lean proteins, and dairy products (if tolerated). Parents should also be mindful of potential nutrient gaps, as a gluten-free diet can sometimes be low in fiber, iron, and B vitamins. Consulting with a pediatric dietitian can help ensure that the child’s diet is well-rounded and meets their nutritional needs.
Challenges and Considerations for Families
Managing gluten sensitivity in children can be challenging for families, particularly when it comes to food preparation, meal planning, and social situations. One of the main concerns is ensuring that the child has access to safe food at home, at school, and during social events. Parents may need to prepare gluten-free meals in advance or educate caregivers, teachers, and friends about the child’s dietary restrictions. Social challenges may also arise, especially when children are invited to birthday parties, school lunches, or other group activities where gluten-containing foods are present. Families may need to bring their own gluten-free options to these events to ensure their child is included. Additionally, cross-contamination in shared kitchens and restaurants can be a concern, and families must take precautions to prevent accidental exposure to gluten.
Support for Parents and Caregivers
Support for parents and caregivers of children with gluten sensitivity is vital for navigating the challenges associated with the condition. It can be helpful to connect with support groups, both in person and online, where parents can share experiences, advice, and resources. These groups often provide emotional support and practical tips for managing gluten sensitivity in children. Pediatricians, dietitians, and other healthcare professionals also play a crucial role in offering guidance on managing the condition and ensuring that the child’s diet is nutritionally adequate. Many families also find it beneficial to join local or national organizations focused on gluten sensitivity or celiac disease, which provide valuable information, advocacy, and resources for families. With the right support, parents and caregivers can ensure that children with gluten sensitivity live healthy, fulfilling lives.
Current Research and Future Directions
The field of gluten sensitivity has seen growing interest in recent years, with numerous studies exploring the condition’s underlying mechanisms, prevalence, and potential treatments. While much progress has been made, there is still a need for more research to better understand gluten sensitivity and its impact on health. As science advances, new diagnostic tools, therapies, and management strategies are emerging, offering hope for individuals living with the condition. Current research is focused on understanding the biological mechanisms of gluten sensitivity, investigating potential treatments, and improving diagnosis to better manage this complex condition.
Recent Studies on Gluten Sensitivity
Recent studies have aimed to clarify the nature of gluten sensitivity, particularly in distinguishing it from other gluten-related disorders like celiac disease and wheat allergy. Researchers are exploring the prevalence of non-celiac gluten sensitivity (NCGS) and its relationship to various gastrointestinal and extra-intestinal symptoms. Some studies suggest that gluten sensitivity may involve immune system activation or sensitivity to other proteins in wheat, in addition to gluten itself. Other research focuses on the role of the gut microbiome in gluten sensitivity, with the possibility that an imbalance in gut bacteria may contribute to the development or exacerbation of symptoms. Although the scientific community continues to debate the causes and mechanisms of gluten sensitivity, these studies provide valuable insights into the condition’s complexity.
Advances in Understanding the Condition
Significant advances have been made in understanding the biological mechanisms behind gluten sensitivity. For example, some studies have identified potential immune responses that might explain why some individuals react to gluten despite not having celiac disease. Recent research has also shed light on how gluten sensitivity may affect not only the digestive system but also other body systems, including the nervous system, joints, and skin. Additionally, advancements in biomarker identification may eventually lead to more reliable diagnostic tests for gluten sensitivity. Researchers are exploring how specific biomarkers related to inflammation and immune system activation could be used to detect gluten sensitivity in the future, offering a more objective and accurate means of diagnosis.
Potential Treatments or Therapies Under Investigation
While the primary treatment for gluten sensitivity remains a strict gluten-free diet, there is ongoing research into potential alternative therapies that could offer relief for individuals with the condition. Some studies are investigating drugs or treatments that could block the inflammatory responses triggered by gluten exposure, reducing symptoms without requiring a complete elimination of gluten from the diet. Additionally, researchers are exploring enzyme-based therapies that could break down gluten in the digestive system before it causes an immune reaction. Other potential therapies under investigation include probiotics and prebiotics, which may help modulate the gut microbiome and reduce inflammation associated with gluten sensitivity. Although these therapies are still in the early stages, they offer promise for improving the management of the condition.
The Future of Gluten Sensitivity Diagnosis and Management
As research progresses, the future of gluten sensitivity diagnosis and management is likely to evolve. The development of accurate diagnostic tests, including blood tests or genetic markers, could make it easier to identify gluten sensitivity and differentiate it from other disorders with similar symptoms. This would help eliminate the need for an exclusionary diagnosis and provide individuals with a more definitive answer to their condition. Additionally, the future may see improvements in treatment options beyond dietary restrictions. Therapies that target the underlying mechanisms of gluten sensitivity, such as immune modulation or gut microbiome regulation, could provide individuals with greater flexibility in managing the condition. As understanding of gluten sensitivity grows, the management of the condition will likely become more personalized and effective, improving quality of life for those affected.
Conclusion
Gluten sensitivity is a complex condition that affects many individuals worldwide, often leading to a variety of digestive, neurological, and systemic symptoms. While its exact cause remains the subject of ongoing research, understanding the nature of gluten sensitivity, its symptoms, and how to manage it effectively can greatly improve the quality of life for those affected. As research continues to uncover more about gluten sensitivity, awareness and proper management will be key to ensuring that individuals can live healthy, fulfilling lives despite their dietary restrictions.
Recap of Key Points About Gluten Sensitivity
Gluten sensitivity, also known as non-celiac gluten sensitivity (NCGS), is a condition in which individuals experience adverse symptoms after consuming gluten, despite not having celiac disease or a wheat allergy. Common symptoms include digestive issues, headaches, fatigue, and skin rashes. Although there are no definitive diagnostic tests for gluten sensitivity, it is typically diagnosed by excluding other conditions and evaluating symptoms. The primary treatment for gluten sensitivity is a gluten-free diet, which can be highly effective in alleviating symptoms. However, individuals with gluten sensitivity must be vigilant about avoiding gluten-containing foods and managing cross-contamination in their daily lives.
Encouraging Awareness and Proper Management
Increasing awareness about gluten sensitivity is essential for ensuring that individuals receive the proper diagnosis and care. Many people who suffer from gluten sensitivity may go undiagnosed or misdiagnosed, which can delay treatment and prolong discomfort. It is crucial for healthcare providers, patients, and families to work together to identify the condition and develop an effective management plan. A gluten-free diet remains the cornerstone of treatment, but it is important to consider other aspects of management, such as ensuring nutritional balance, managing mental health, and providing support for those living with gluten sensitivity. Education and resources for patients, caregivers, and medical professionals will help ensure that people with gluten sensitivity lead healthy, active lives.
Final Thoughts on Living with Gluten Sensitivity
Living with gluten sensitivity requires adaptation, but it is entirely possible to thrive with the right support and lifestyle adjustments. Though it can be challenging at times, individuals with gluten sensitivity can lead fulfilling lives by being proactive about their health, advocating for themselves in social situations, and relying on a strong support network. With ongoing research, advancements in diagnosis and treatment, and a growing understanding of the condition, the future for individuals with gluten sensitivity looks promising. By staying informed, committed to proper management, and sharing experiences with others, those living with gluten sensitivity can overcome obstacles and maintain a positive outlook.