The Brain’s Emergency Call
The brain is the most vital organ of the body, controlling everything from breathing to decision-making. But what happens when it faces a sudden, life-threatening event? A stroke is often referred to as the brain’s “emergency call,” and understanding it can save lives. Let’s explore what a stroke is, why time is critical, and the surprising reality that strokes can strike anyone, regardless of age.
What is a Stroke?
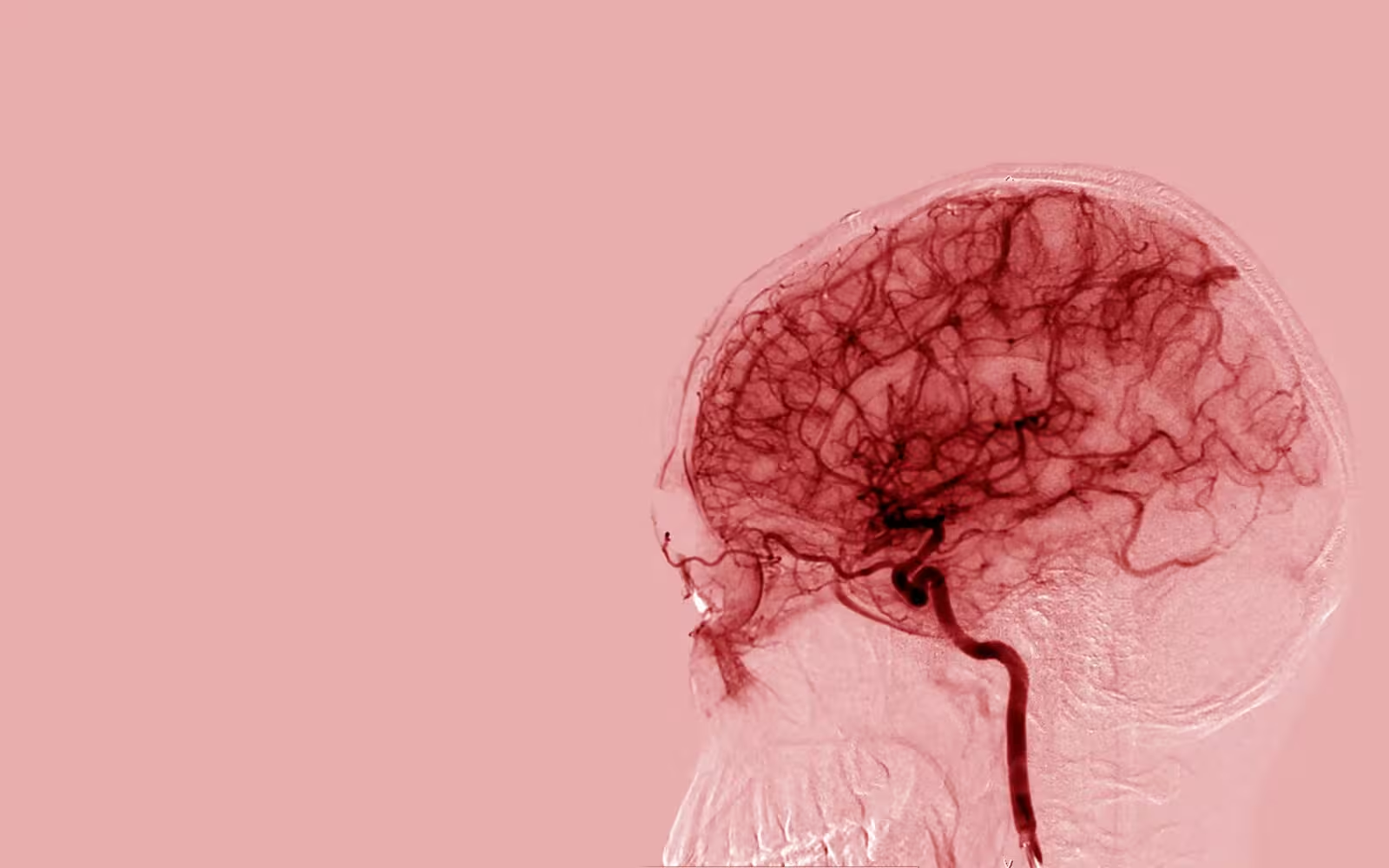
A stroke occurs when blood flow to a part of the brain is interrupted or significantly reduced. Without an adequate blood supply, brain cells begin to die within minutes, causing potential permanent damage. Strokes can be caused by either a blockage (ischemic stroke) or the rupture of a blood vessel (hemorrhagic stroke).
The brain requires a constant flow of oxygen and nutrients to function. When this flow is disrupted, it’s like a power outage, and the consequences can range from temporary weakness to severe disability or even death. Recognizing the symptoms early, such as sudden numbness, difficulty speaking, or blurred vision, is key to minimizing its impact.
Why Every Second Matters
Time is the most critical factor during a stroke. Medical professionals often say, “Time lost is brain lost,” meaning the longer the brain goes without oxygen, the more irreversible the damage.
Treatments like clot-busting medications (for ischemic strokes) are only effective if administered within a specific time window, typically 3 to 4.5 hours from the onset of symptoms. Delays in seeking medical attention can mean the difference between recovery and permanent disability.
Quick action, such as calling emergency services immediately upon noticing symptoms, can save not just the person’s life but also their quality of life. This urgency emphasizes the importance of public awareness about recognizing stroke symptoms through tools like the FAST acronym:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call emergency services
A Shocking Truth: Strokes Can Happen at Any Age
Many people think strokes only happen to older adults, but this is a dangerous misconception. While age is a significant risk factor, strokes can affect people of all ages, including infants, children, and young adults.
Certain conditions, such as high blood pressure, diabetes, and heart disorders, can predispose anyone to a stroke. Additionally, lifestyle factors like smoking, obesity, and lack of physical activity are increasing stroke incidences in younger populations. Rare causes, such as genetic blood clotting disorders or trauma, can also lead to strokes in seemingly healthy individuals.
This reality underlines the importance of preventive care at every age. Regular health check-ups, maintaining a balanced diet, staying active, and managing stress are critical steps in reducing the risk of a stroke.
Types of Stroke: The Culprits Revealed
A stroke is a devastating event, but understanding its types can illuminate the causes and improve prevention and treatment strategies. Each type of stroke acts as a unique culprit, with distinct mechanisms and risks. Let’s uncover the main types: ischemic strokes, hemorrhagic strokes, and transient ischemic attacks (TIAs), or “mini-strokes.”
The Chokehold (Ischemic Stroke)
The most common type of stroke, an ischemic stroke, occurs when blood flow to the brain is blocked, often compared to a chokehold. This type accounts for nearly 87% of all strokes, emphasizing the importance of understanding its mechanisms and causes.
When Blood Flow Halts
An ischemic stroke happens when a blood vessel carrying oxygen-rich blood to the brain becomes obstructed. The obstruction can occur due to a blood clot (thrombus) forming directly in the brain’s vessels or an embolism, where a clot or debris travels from elsewhere in the body. Without oxygen and nutrients, brain cells in the affected area start dying rapidly.
Common Causes: The Unseen Villains
Ischemic strokes often arise from underlying health conditions or lifestyle factors. Common culprits include:
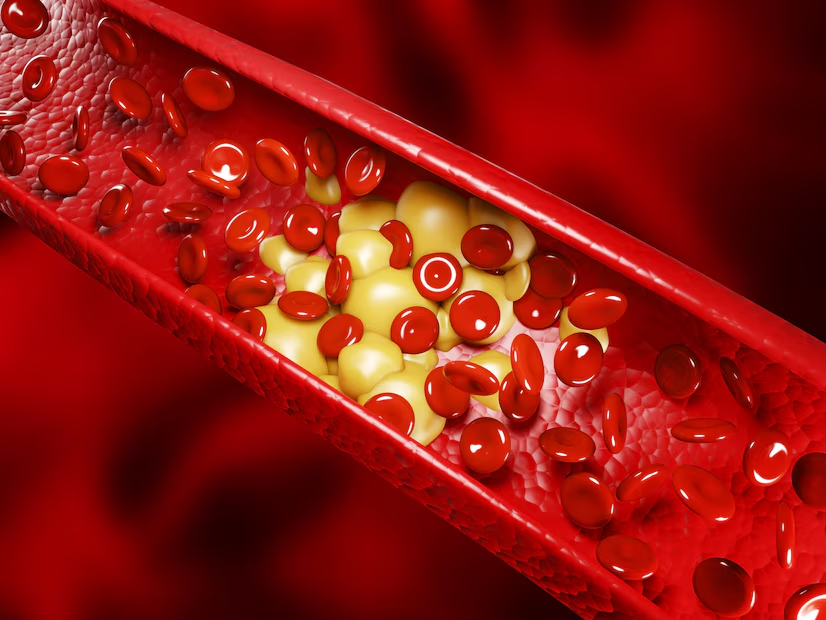
- Atherosclerosis: The buildup of fatty deposits in the arteries narrows blood flow.
- Atrial Fibrillation: An irregular heart rhythm that can lead to clot formation.
- Smoking: Damages blood vessels and accelerates clot formation.
- High Cholesterol: Increases the risk of arterial blockages.
Preventive measures, such as managing blood pressure and cholesterol and avoiding smoking, are essential to reduce the risk of an ischemic stroke.
The Burst (Hemorrhagic Stroke)
Unlike ischemic strokes, hemorrhagic strokes are caused by bleeding in the brain, making it a violent and catastrophic event. Known as the “burst,” this type of stroke has a lower occurrence rate but often more severe outcomes.
Blood Vessels Under Siege
A hemorrhagic stroke occurs when a weakened blood vessel ruptures, spilling blood into or around the brain. This bleeding increases pressure inside the skull, damaging brain tissue. The two primary types of hemorrhagic strokes are:
- Intracerebral Hemorrhage: Bleeding occurs directly within the brain tissue.
- Subarachnoid Hemorrhage: Bleeding happens in the space between the brain and the thin tissues covering it.
High-Pressure Risks and Red Flags
The primary risk factor for hemorrhagic strokes is high blood pressure, which puts immense strain on blood vessel walls. Other risks include:
- Aneurysms: Bulges in blood vessels that can burst.
- Head Injuries: Traumatic damage to blood vessels.
- Blood Thinners: Medications that increase bleeding risk.
Symptoms like sudden severe headache, nausea, or loss of consciousness should be treated as medical emergencies, as time is critical in managing hemorrhagic strokes.
The Warning Whisper (TIA)
A transient ischemic attack (TIA), or “mini-stroke,” serves as a warning whisper from the body—a brief interruption in blood flow that resolves quickly but signals serious danger ahead.
Mini-Stroke, Major Warning
While symptoms of a TIA mirror those of a stroke—weakness, slurred speech, or vision loss—they typically last only a few minutes to an hour and do not cause permanent damage. This often leads people to dismiss them, but TIAs are anything but trivial.
The Danger Lurking Ahead
A TIA is often a precursor to a major stroke. Statistics show that approximately 1 in 3 people who experience a TIA will go on to have a stroke, often within days or weeks. The causes of TIAs are similar to ischemic strokes, including clots or narrowed arteries.
Immediate medical evaluation after a TIA can help identify underlying risks and implement preventive measures, such as medication or surgical intervention to restore proper blood flow.
The Unseen Prelude: Risk Factors
A stroke doesn’t happen out of the blue—it’s often the result of an unseen prelude of risk factors building up over time. These risk factors can range from well-known culprits like hypertension to less obvious ones like stress and genetics. Let’s delve into the “ticking time bombs” and the “unexpected triggers” that pave the way for this brain emergency.
Ticking Time Bombs
Some risk factors for stroke are so common they’re often overlooked, yet they act as silent threats, ticking away until a crisis strikes. These include conditions and habits that are preventable or manageable with the right interventions.
Hypertension: The Silent Killer
High blood pressure is the leading risk factor for strokes. It exerts constant pressure on the walls of blood vessels, weakening them over time and increasing the likelihood of both ischemic and hemorrhagic strokes. Many people are unaware they have hypertension until it’s too late, which is why routine monitoring is essential.
Diabetes: A Double Threat
Diabetes doubles the risk of a stroke. High blood sugar levels damage blood vessels and accelerate atherosclerosis (the narrowing and hardening of arteries). Additionally, diabetes is often accompanied by other risk factors like high cholesterol and hypertension, creating a dangerous cocktail for stroke risk.
Smoking: Poison for Your Arteries
Smoking introduces harmful chemicals into the bloodstream that damage blood vessels, increase clot formation, and reduce oxygen supply to the brain. Even exposure to secondhand smoke can elevate the risk. Quitting smoking can significantly lower the chance of a stroke, regardless of age or smoking history.
The Unexpected Triggers
While some risk factors are more obvious, others are unexpected and often underestimated. These triggers can sneak up on individuals, catching them unprepared.
Stress: The Underestimated Adversary
Chronic stress increases the production of cortisol, a hormone that can lead to elevated blood pressure, inflammation, and blood clotting issues. Stress also encourages unhealthy coping mechanisms like overeating, smoking, or neglecting physical activity—all of which increase stroke risk.
Genetics: A Family History of Risk
Your DNA can play a significant role in your stroke risk. A family history of stroke or cardiovascular disease may indicate a genetic predisposition to conditions like high blood pressure, high cholesterol, or clotting disorders. While you can’t change your genes, being aware of your family history can help guide preventive measures.
Silent Heart Conditions: Hidden Hazards
Heart disorders like atrial fibrillation (AFib) and valvular heart disease often operate in the shadows, causing no symptoms until they lead to serious complications like a stroke. AFib, for instance, increases stroke risk by five times because it allows blood clots to form in the heart and travel to the brain. Regular heart health check-ups are crucial for detecting and managing these hidden risks.
By understanding the ticking time bombs and unexpected triggers behind strokes, we can take proactive steps to mitigate risk. Early detection, lifestyle changes, and medical interventions can transform these unseen preludes into opportunities for prevention and protection.
Signs of Stroke: Decoding the SOS
When a stroke strikes, the brain sends out an urgent SOS in the form of symptoms. Recognizing these warning signs quickly can save lives and prevent long-term damage. However, not all symptoms are obvious. Here, we’ll explore the BE FAST method to identify stroke signs and discuss the silent, atypical symptoms that are easy to miss.
BE FAST
Stroke symptoms often appear suddenly, and using the BE FAST acronym is an effective way to spot them and act immediately. Each letter represents a critical symptom to look for and serves as a reminder to seek help without delay.
How to Recognize the Signs
- Balance: Sudden loss of balance or coordination. The person may feel dizzy or unable to stand steadily.
- Eyes: Sudden changes in vision, such as blurriness, double vision, or loss of vision in one or both eyes.
- Face: Noticeable drooping on one side of the face. Ask the person to smile; if their smile is uneven, it’s a red flag.
- Arms: Sudden weakness or numbness in one arm. Ask the person to raise both arms; if one drifts downward, it could indicate a stroke.
- Speech: Slurred or garbled speech, or an inability to speak. Ask the person to repeat a simple sentence, like “The sky is blue.” If they struggle, it’s time to act.
- Time: Time is critical. If you notice any of these signs, call emergency services immediately. The faster medical help is given, the better the chances of recovery.
The Silent Symptoms
While BE FAST covers the most common and obvious signs of stroke, not all strokes present the same way. Some symptoms are subtler and may be mistakenly attributed to other conditions. Knowing these silent symptoms can help catch strokes that might otherwise go unnoticed.
Atypical Signs You Might Overlook
- Sudden Severe Headache: A sharp, intense headache that appears without warning could indicate a hemorrhagic stroke, especially if accompanied by nausea or vomiting.
- Unexplained Fatigue or Confusion: Feeling suddenly and inexplicably tired, dazed, or confused may be an early stroke symptom, particularly in women.
- Hiccups or Chest Pain: These unusual symptoms, particularly in women, can indicate a stroke affecting the brain stem.
- Facial Numbness Without Drooping: Tingling or numbness on one side of the face, even if it doesn’t droop, can still signal a stroke.
- Difficulty Swallowing or Breathing: Sudden trouble swallowing or shortness of breath may indicate a stroke in specific areas of the brain.
Silent symptoms are often dismissed or attributed to fatigue, dehydration, or stress. However, if they appear suddenly and are severe, they shouldn’t be ignored.
The Importance of Acting Fast
Even with mild or atypical symptoms, every second counts. Brain cells begin to die within minutes of a stroke, and immediate medical intervention can significantly improve outcomes. Knowing both the BE FAST method and the less obvious signs equips you to recognize the brain’s SOS and respond effectively.
Stroke Through the Ages
Stroke is often perceived as a condition of the elderly, but the reality is that it can strike at any age. From young adults to seniors, each age group faces unique risk factors and challenges. Understanding how stroke affects different age groups helps debunk myths and emphasizes the importance of awareness and prevention for everyone.
Young and Struck
Many people believe strokes only happen in older adults, but this misconception overlooks a growing trend—strokes among younger individuals. Young adults, teenagers, and even children can experience strokes, and the implications are profound.
Why Strokes Aren’t Just for the Elderly
The rise in strokes among younger populations is attributed to a combination of factors:
- Lifestyle Choices: Poor diets, smoking, excessive alcohol consumption, and sedentary habits are becoming more prevalent in younger age groups.
- Chronic Conditions: High blood pressure, diabetes, and obesity are no longer just concerns for older individuals; they are now affecting people in their 20s and 30s.
- Birth-Related Factors: In children and infants, strokes can result from complications during birth, congenital heart defects, or rare blood disorders.
- Rare Causes: Traumatic injuries, such as head trauma or neck artery tears, can lead to strokes even in active, healthy individuals.
The Impact on Younger Lives
Strokes in young adults often occur during their most productive years, affecting careers, families, and futures. The long-term impact can include significant physical, emotional, and financial challenges. However, younger patients also have better recovery potential due to greater brain plasticity, provided they receive timely treatment.
Golden Years and Risks
While younger individuals are not immune, advancing age remains one of the most significant risk factors for stroke. Seniors are more vulnerable due to age-related changes in the body and cumulative exposure to risk factors over time.
Age-Related Vulnerabilities
- Weakened Blood Vessels: As people age, their blood vessels lose elasticity and become more prone to blockages or ruptures, increasing the risk of both ischemic and hemorrhagic strokes.
- Chronic Health Conditions: Conditions like atrial fibrillation, high blood pressure, and high cholesterol are more common in older adults, heightening stroke risks.
- Cognitive Decline: Dementia and cognitive impairments can mask early stroke symptoms, delaying diagnosis and treatment.
- Impaired Mobility: Reduced physical activity in older age contributes to poorer cardiovascular health, compounding stroke risks.
A Call for Vigilance
For seniors, preventive care is vital. Regular health check-ups, managing chronic conditions, and staying active can significantly reduce stroke risk. Families and caregivers should also educate themselves about stroke symptoms, as older adults may not recognize or report them promptly.
Stroke Through the Ages
Stroke is often perceived as a condition of the elderly, but the reality is that it can strike at any age. From young adults to seniors, each age group faces unique risk factors and challenges. Understanding how stroke affects different age groups helps debunk myths and emphasizes the importance of awareness and prevention for everyone.
Young and Struck
Many people believe strokes only happen in older adults, but this misconception overlooks a growing trend—strokes among younger individuals. Young adults, teenagers, and even children can experience strokes, and the implications are profound.
Why Strokes Aren’t Just for the Elderly
The rise in strokes among younger populations is attributed to a combination of factors:
- Lifestyle Choices: Poor diets, smoking, excessive alcohol consumption, and sedentary habits are becoming more prevalent in younger age groups.
- Chronic Conditions: High blood pressure, diabetes, and obesity are no longer just concerns for older individuals; they are now affecting people in their 20s and 30s.
- Birth-Related Factors: In children and infants, strokes can result from complications during birth, congenital heart defects, or rare blood disorders.
- Rare Causes: Traumatic injuries, such as head trauma or neck artery tears, can lead to strokes even in active, healthy individuals.
The Impact on Younger Lives
Strokes in young adults often occur during their most productive years, affecting careers, families, and futures. The long-term impact can include significant physical, emotional, and financial challenges. However, younger patients also have better recovery potential due to greater brain plasticity, provided they receive timely treatment.
Golden Years and Risks
While younger individuals are not immune, advancing age remains one of the most significant risk factors for stroke. Seniors are more vulnerable due to age-related changes in the body and cumulative exposure to risk factors over time.
Age-Related Vulnerabilities
- Weakened Blood Vessels: As people age, their blood vessels lose elasticity and become more prone to blockages or ruptures, increasing the risk of both ischemic and hemorrhagic strokes.
- Chronic Health Conditions: Conditions like atrial fibrillation, high blood pressure, and high cholesterol are more common in older adults, heightening stroke risks.
- Cognitive Decline: Dementia and cognitive impairments can mask early stroke symptoms, delaying diagnosis and treatment.
- Impaired Mobility: Reduced physical activity in older age contributes to poorer cardiovascular health, compounding stroke risks.
A Call for Vigilance
For seniors, preventive care is vital. Regular health check-ups, managing chronic conditions, and staying active can significantly reduce stroke risk. Families and caregivers should also educate themselves about stroke symptoms, as older adults may not recognize or report them promptly.
The Aftermath: Life After a Stroke
A stroke is a life-altering event that doesn’t end with emergency treatment. The aftermath brings its own challenges, encompassing physical, emotional, and cognitive struggles. Understanding what comes after a stroke can help survivors and their loved ones navigate the recovery process and adapt to a new normal.
The Recovery Journey
Recovery after a stroke is often long and complex, requiring a combination of medical treatment, rehabilitation, and personal determination. While every survivor’s journey is unique, most share common steps in rebuilding their lives.
Rehabilitation and Therapy
Rehabilitation is a cornerstone of stroke recovery, designed to help survivors regain lost abilities and adapt to new limitations. It focuses on improving mobility, speech, and daily living skills.
- Physical Therapy: Aims to restore movement, strength, and coordination, often addressing issues like paralysis or muscle weakness. Exercises are tailored to the survivor’s specific needs.
- Occupational Therapy: Helps survivors relearn essential tasks like dressing, cooking, and using technology, fostering independence in daily life.
- Speech Therapy: Assists those who struggle with speech, language, or swallowing due to stroke-related brain damage. Therapists use exercises to improve communication and cognitive skills.
- Assistive Devices: Mobility aids like canes, wheelchairs, or orthotics play a critical role in supporting independence during recovery.
Rehabilitation is most effective when started early and pursued consistently. Support from healthcare providers, caregivers, and family is crucial in maintaining motivation and progress.
Emotional and Cognitive Battles
While physical recovery often takes center stage, the emotional and cognitive challenges of life after a stroke are equally significant. These hidden battles can profoundly impact the survivor’s quality of life and overall recovery.
Dealing with Depression and Memory Loss
- Depression and Anxiety:
Depression is a common aftermath of a stroke, affecting nearly one-third of survivors. It stems from changes in brain chemistry, frustration over physical limitations, and fear of future strokes. Signs include persistent sadness, fatigue, and loss of interest in activities. Anxiety may also arise from fear of recurrence or struggles with dependence.- Management: Professional counseling, medication, and support groups can help stroke survivors cope with these feelings. Encouragement from family and friends is vital.
- Memory Loss and Cognitive Impairment:
Many stroke survivors face difficulties with memory, attention, and problem-solving. These challenges can make it hard to manage daily tasks, hold conversations, or return to work.- Management: Cognitive therapy, memory exercises, and tools like reminders or planners can assist survivors in adapting to these changes. Patience and understanding from caregivers can ease the adjustment process.
Building Emotional Resilience
Overcoming these challenges requires emotional resilience, which can be nurtured through:
- Support Networks: Family, friends, and stroke survivor communities provide comfort and shared experiences.
- Positive Reinforcement: Celebrating small victories fosters confidence and optimism.
- Mindfulness and Relaxation: Techniques like meditation or yoga can reduce stress and improve emotional well-being.
Prevention: Your Brain’s Shield
Preventing a stroke is far easier and more effective than treating one. By adopting proactive measures, you can shield your brain and overall health from this life-threatening event. Prevention is built on two pillars: a healthy lifestyle and medical vigilance. Let’s explore how these strategies can fortify your brain’s defenses.
Lifestyle Makeover
Your daily habits play a significant role in determining your stroke risk. A healthy lifestyle isn’t just a suggestion; it’s a necessity for long-term well-being. Small changes in diet, exercise, and stress management can have a massive impact.
Diet, Exercise, and Stress Management
- Diet:
Nutrition is the cornerstone of stroke prevention. Eating the right foods can help maintain healthy blood pressure, cholesterol levels, and weight—all critical factors in reducing stroke risk.- What to Eat: Focus on a Mediterranean-style diet rich in fruits, vegetables, whole grains, lean proteins (like fish and chicken), and healthy fats (like olive oil and nuts).
- What to Avoid: Cut back on processed foods, excess salt, sugary drinks, and trans fats, all of which contribute to high blood pressure and obesity.
- Hydration: Drink plenty of water, as dehydration can affect blood flow and increase clotting risk.
- Exercise:
Regular physical activity strengthens your cardiovascular system, lowers blood pressure, and reduces stress. Aim for at least 30 minutes of moderate exercise most days of the week.- Cardio: Activities like walking, swimming, or cycling boost heart health.
- Strength Training: Building muscle improves overall metabolism and blood sugar control.
- Consistency Matters: The key is making exercise a habit, not a chore.
- Stress Management:
Chronic stress takes a toll on your cardiovascular system, increasing the risk of stroke. Learning to manage stress can lower blood pressure and improve mental health.- Mindfulness Techniques: Practices like meditation, deep breathing, or yoga can help you stay calm.
- Time Management: Avoid overloading your schedule and prioritize self-care.
- Seek Support: Talking to a therapist or loved one can help alleviate stress.
Medical Must-Dos
While lifestyle changes are critical, they should be paired with medical vigilance. Regular checkups and adhering to prescribed treatments are essential components of stroke prevention.
Regular Checkups and Medication Adherence
- Regular Health Screenings:
Routine checkups allow doctors to monitor and manage key risk factors like blood pressure, cholesterol, and blood sugar levels.- Blood Pressure: High blood pressure is the leading cause of strokes. Check it regularly and keep it under control.
- Cholesterol Levels: Elevated LDL (“bad” cholesterol) contributes to atherosclerosis, increasing stroke risk.
- Blood Sugar: Diabetes significantly raises stroke risk, so regular monitoring is vital.
- Medication Adherence:
If you’ve been prescribed medications for conditions like hypertension, diabetes, or high cholesterol, taking them as directed is non-negotiable. Skipping doses or stopping medication can dangerously elevate stroke risk.- Blood Thinners: For some, medications like aspirin or anticoagulants help prevent clot formation.
- Medication Tracking: Use reminders or pill organizers to ensure you don’t miss doses.
- Vaccinations and Preventive Care:
Staying up-to-date on vaccines and addressing underlying infections or conditions promptly can further reduce your risk.
The Power of Prevention
Taking charge of your lifestyle and staying on top of medical care creates a powerful shield against stroke. While no one can completely eliminate risk, these measures significantly lower the odds and empower you to live a healthier, more vibrant life. Prevention is your brain’s ultimate shield—start building it today.
Debunking Stroke Myths
Stroke is a leading cause of death and disability worldwide, yet misconceptions about it persist, often preventing timely action and effective prevention. Separating fact from fiction is essential to safeguard lives and promote awareness. Let’s unravel some common myths that put lives at risk.
Common Misconceptions That Put Lives at Risk
Myth 1: Strokes Only Happen to the Elderly
Reality: While age is a significant risk factor, strokes can strike at any age. In fact, an increasing number of young adults, teenagers, and even children are experiencing strokes due to lifestyle changes, genetics, or underlying medical conditions. Believing strokes are an “older person’s problem” can lead younger individuals to ignore symptoms or skip preventive measures.
Myth 2: Strokes Are Rare
Reality: Strokes are far more common than many people think. According to the World Stroke Organization, one in four adults over the age of 25 will have a stroke in their lifetime. This widespread condition demands awareness, not complacency.
Myth 3: Strokes Can’t Be Prevented
Reality: Up to 80% of strokes are preventable with the right lifestyle choices and medical care. Controlling blood pressure, maintaining a healthy weight, quitting smoking, and managing chronic conditions like diabetes or high cholesterol can dramatically reduce risk.
Myth 4: If Symptoms Go Away, It’s Nothing Serious
Reality: Temporary stroke symptoms, such as weakness or vision loss that resolve quickly, may indicate a transient ischemic attack (TIA), also known as a “mini-stroke.” TIAs are major warning signs of a future stroke. Ignoring them could lead to severe consequences, as one in three people with a TIA will have a full-blown stroke later.
Myth 5: Strokes Are Painless
Reality: Not all strokes are painless. While some may cause sudden numbness or paralysis without discomfort, others, particularly hemorrhagic strokes, can trigger excruciating headaches, neck pain, or vomiting. Assuming a stroke is painless can delay recognizing life-threatening symptoms.
Myth 6: You Can Wait Out Stroke Symptoms
Reality: Time is critical during a stroke. The phrase “time is brain” reflects the fact that millions of brain cells die every minute without treatment. Immediate medical attention is essential, as clot-busting medications or surgical interventions can only be administered within specific time windows.
Myth 7: Stroke Recovery Is Impossible
Reality: While strokes can leave lasting effects, many survivors make significant recoveries with rehabilitation and therapy. Physical, occupational, and speech therapies, along with a supportive environment, can help rebuild lost abilities and improve quality of life.
Myth 8: Strokes Always Affect the Heart
Reality: A stroke is a brain event, not a heart event. It occurs when blood flow to the brain is disrupted. Confusing strokes with heart attacks can lead to delays in seeking appropriate care and treatment.
Myth 9: Men Are More Likely to Have Strokes Than Women
Reality: Women are actually at a slightly higher risk of stroke than men, and they are more likely to die from one. Hormonal factors, pregnancy, and longer life expectancy contribute to women’s increased vulnerability. This myth can lead to overlooked risks and symptoms in women.
Myth 10: You Can’t Do Anything Once a Stroke Starts
Reality: Acting fast is crucial. Recognizing the BE FAST signs—Balance, Eyes, Face, Arms, Speech, and Time—can make the difference between recovery and severe disability or death. Calling emergency services immediately ensures that treatment begins as quickly as possible.
Real Stories, Real Lessons
Stroke is a powerful and often unpredictable event, but many survivors prove that resilience, determination, and hope can lead to remarkable recoveries. Through their stories, we gain valuable insights into the importance of early action, the impact of rehabilitation, and the strength of the human spirit. Let’s explore some inspiring accounts of stroke survivors and the lessons they teach us.
Inspiring Accounts of Survivors
1. John’s Journey: From Paralysis to Independence
John, a 45-year-old father of two, had no prior health issues when he suddenly collapsed at work. His coworkers quickly recognized the signs of a stroke and called emergency services immediately. John was diagnosed with an ischemic stroke, which left him paralyzed on his left side.
The Recovery Journey:
John’s recovery was long and grueling, filled with months of physical therapy and occupational therapy. At first, simple tasks like eating, dressing, and walking were impossible. But John never lost hope. He was determined to regain independence and be there for his children.
The Lesson:
John’s story teaches us the critical importance of recognizing stroke symptoms and seeking help immediately. His recovery was also a testament to the power of physical therapy and the body’s ability to heal with dedication and perseverance. Early intervention and consistent rehabilitation are vital for recovery.
2. Mary’s Story: Overcoming a Silent Stroke
Mary, a 60-year-old retired teacher, experienced a stroke while out for a walk. Initially, she had no obvious symptoms—just a subtle tingling sensation in her left arm and mild dizziness. She dismissed it as fatigue and didn’t seek immediate medical attention. Later, her husband noticed her speech was slurred and her face appeared slightly droopy. By the time they reached the hospital, Mary had suffered significant cognitive impairments, including memory loss and difficulty speaking.
The Recovery Journey:
Mary’s stroke was classified as a silent stroke, a condition where brain damage occurs without immediate, visible symptoms. Despite the challenges, Mary’s doctors started a comprehensive rehabilitation plan that included speech therapy and cognitive exercises. It was a slow road, but Mary gradually regained her speech and memory, eventually returning to a fulfilling life of volunteer work and spending time with her family.
The Lesson:
Mary’s experience highlights the importance of not ignoring even mild or seemingly insignificant symptoms. Her story also emphasizes that silent strokes can lead to major cognitive impairments, and the recovery process can be lengthy. Patience and persistence, combined with early medical intervention, are key to regaining functionality.
3. Tom’s Triumph: A Survivor’s Unexpected Second Chance
Tom, a 35-year-old lawyer, suffered a stroke while on vacation with his family. A healthy, active man with no history of medical issues, Tom was shocked when he suddenly felt a sharp headache followed by numbness in his right arm and leg. His wife immediately called an ambulance, and Tom was rushed to the hospital where doctors diagnosed him with a severe ischemic stroke.
The Recovery Journey:
Tom’s rehabilitation journey was intense and filled with setbacks. After months of physical therapy, speech therapy, and emotional support, Tom was able to return to his work and even became an advocate for stroke awareness, sharing his story to help others. Tom also adopted a healthier lifestyle, including regular exercise and a balanced diet, to reduce his stroke risk moving forward.
The Lesson:
Tom’s story demonstrates that stroke can affect anyone, regardless of age or lifestyle. His recovery also shows the profound impact of emotional resilience and social support in overcoming challenges. The journey to recovery isn’t always linear, but with determination and commitment to rehabilitation, progress is possible.
4. Samantha’s Story: A Stroke at 28
Samantha, a 28-year-old marketing professional, experienced a stroke while preparing for a big presentation at work. She suddenly felt dizzy, and her left side went numb. Thinking it was just stress, she brushed it off at first. However, as her speech became slurred and she struggled to stand, her coworkers called for help, and she was rushed to the hospital. Doctors determined that she had a clot-induced ischemic stroke.
The Recovery Journey:
After receiving immediate medical treatment, Samantha underwent intensive physical therapy and learning to speak again. Despite being young and otherwise healthy, her stroke left lasting effects, including challenges with fine motor skills and some memory difficulties. Through perseverance, therapy, and a strong support network, Samantha regained much of her previous function.
The Lesson:
Samantha’s story highlights that strokes don’t discriminate by age. It also underscores the importance of recognizing and acting on symptoms quickly. Her experience also shows how recovery is not just about physical health, but also emotional support, which plays a crucial role in regaining confidence and functionality after a stroke.
5. David’s Determination: A Stroke Survivor’s Advocacy
David, a 50-year-old engineer, had a stroke caused by high blood pressure. He didn’t realize the importance of managing his condition until it was too late. After being hospitalized, David spent several months undergoing rehabilitation for his motor skills, vision, and speech. As part of his recovery, he became an advocate for stroke awareness, sharing his journey to help others understand the importance of prevention.
The Recovery Journey:
David’s rehabilitation focused on physical and speech therapy, along with lifestyle changes like medication management and regular exercise. His recovery wasn’t immediate, but with time, he returned to work and started spreading awareness about stroke prevention and healthy living.
The Lesson:
David’s story emphasizes the importance of managing risk factors like high blood pressure and the role that education and advocacy can play in preventing strokes. His work in raising awareness helped others understand that stroke prevention starts with knowing your health risks and taking action to mitigate them.
A Call to Action
Stroke is a leading cause of death and disability worldwide, but it doesn’t have to be. The power to reduce stroke mortality lies in early intervention, community awareness, and proactive prevention. By coming together as a society, we can ensure that more lives are saved, more people recover fully, and fewer strokes occur. It starts with you.
The Power of Early Response and Community Awareness
The key to minimizing the devastating impact of stroke is rapid recognition and timely action. When stroke symptoms are identified early, treatments can be administered to save brain tissue, improve outcomes, and prevent disability.
Early Response Saves Lives
A stroke is a medical emergency, and the faster it is treated, the better the chances of survival and recovery. Recognizing stroke symptoms and calling for help immediately can make a life-or-death difference. Knowing the signs of stroke—using the BE FAST acronym—helps people act quickly:
- Balance: Sudden loss of balance or coordination.
- Eyes: Vision problems or sudden loss of vision.
- Face: Facial drooping, especially on one side.
- Arms: Weakness or numbness, especially in one arm.
- Speech: Slurred speech or difficulty speaking.
- Time: Time to call emergency services.
Calling 911 or your local emergency number immediately is crucial for getting professional help fast. Emergency medical teams can administer life-saving treatments such as clot-busting drugs or surgical interventions if the stroke is caught within the critical time window.
Community Awareness: A Collective Responsibility
Creating widespread awareness in communities can help ensure more people understand the signs of stroke and the importance of rapid response. Public education campaigns, health initiatives, and partnerships with local healthcare providers can teach people to recognize the symptoms and respond appropriately. Communities that are educated about stroke can also play a role in prevention by encouraging healthy lifestyle changes and promoting regular health screenings.
Schools, workplaces, and local organizations can hold workshops or distribute materials to raise awareness. By equipping communities with this knowledge, we build a collective safety net that ensures stroke victims receive timely care, and that fewer people experience strokes in the first place.
How You Can Help Reduce Stroke Mortality
You don’t need to be a healthcare professional to make a difference in the fight against stroke. There are practical actions you can take to reduce stroke mortality both in your own life and in your community.
1. Recognize the Symptoms and Act Fast
The most immediate way to help reduce stroke mortality is by recognizing stroke symptoms in yourself or others and acting quickly. If you or someone you know shows signs of a stroke, don’t wait—call for emergency help. Time is critical in minimizing brain damage and maximizing recovery.
2. Advocate for Stroke Awareness
As a member of your community, you have the power to raise awareness about stroke prevention and the importance of early intervention. Share the BE FAST acronym with family, friends, and colleagues. You can help educate people about the risk factors, symptoms, and the life-saving importance of fast action. Participating in stroke awareness events, supporting stroke organizations, or even sharing educational materials on social media are all ways to contribute to the cause.
3. Promote Healthy Lifestyle Choices
Encourage those around you to adopt healthy habits that reduce the risk of stroke, such as:
- Maintaining a balanced diet: Eating more fruits, vegetables, whole grains, and healthy fats, while reducing salt, sugar, and processed foods.
- Regular exercise: Engaging in physical activity at least 30 minutes a day to improve cardiovascular health.
- Avoiding smoking: Smoking damages blood vessels and increases stroke risk.
- Limiting alcohol: Drinking in moderation can help lower stroke risk.
- Managing stress: Practicing stress-reduction techniques like meditation, yoga, or regular breaks from work.
- Getting regular checkups: Having blood pressure, cholesterol, and blood sugar levels monitored can help catch problems early before they lead to stroke.
4. Know Your Risk Factors and Get Screened
Knowing your individual risk factors can help you take action to lower your risk. High blood pressure, diabetes, high cholesterol, and a family history of stroke increase your likelihood of having one. If you’re at risk, talk to your doctor about regular screenings and the steps you can take to manage these conditions.
5. Support Stroke Survivors
Stroke doesn’t just affect the person who suffers it; it impacts their family, friends, and entire community. Supporting stroke survivors as they recover—whether through rehabilitation, emotional support, or simply helping them adapt to new life challenges—makes a significant difference. By offering encouragement and compassion, you help reduce the emotional and psychological toll of stroke, aiding in the recovery process.
6. Be Involved in Stroke Research and Fundraising
Participating in or supporting research into stroke treatment and prevention can help improve survival rates and recovery outcomes for future generations. Fundraising for stroke research organizations or donating to initiatives focused on stroke education and recovery can directly contribute to reducing stroke mortality in the long term.
Conclusion
Reducing stroke mortality is a collective effort that begins with awareness and early response. By recognizing the signs of stroke, encouraging healthy lifestyles, and supporting medical advancements, you can be a part of the movement to reduce the devastating impact of stroke on individuals and communities worldwide. The call to action is clear: when we work together, we can save lives, improve outcomes, and make the world a healthier place for everyone.